Page 42 - ANZCP Gazette APRIL 2022
P. 42
Willcox et al.
7
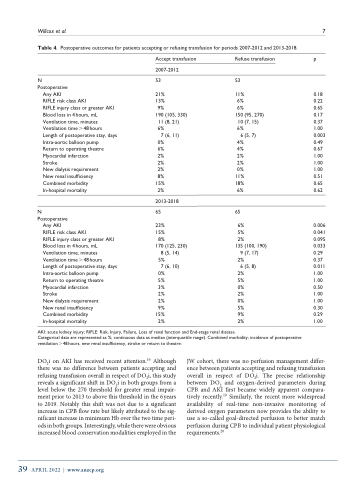
Table 4. Postoperative outcomes for patients accepting or refusing transfusion for periods 2007-2012 and 2013-2018.
N Postoperative
Any AKI
RIFLE risk class AKI
RIFLE injury class or greater AKI Blood loss in 4hours, mL Ventilation time, minutes Ventilation time > 48 hours Length of postoperative stay, days Intra-aortic balloon pump
Return to operating theatre Myocardial infarction
Stroke
New dialysis requirement
New renal insufficiency Combined morbidity
In-hospital mortality
N Postoperative
Any AKI
RIFLE risk class AKI
RIFLE injury class or greater AKI Blood loss in 4hours, mL Ventilation time, minutes Ventilation time > 48 hours Length of postoperative stay, days Intra-aortic balloon pump
Return to operating theatre Myocardial infarction
Stroke
New dialysis requirement
New renal insufficiency Combined morbidity
In-hospital mortality
Accept transfusion 2007-2012
53
21% 13% 9%
190 (105, 330) 11 (8, 21)
6%
7 (6, 11) 0%
6% 2% 2% 2% 8%
15% 2%
2013-2018
65
23% 15% 8%
170 (125, 230) 8 (5, 14)
5%
7 (6, 10)
0% 5% 3% 2% 2% 9%
15% 2%
Refuse transfusion
53
11% 6% 6%
150 (95, 270) 10 (7, 15) 6%
6 (5, 7) 4%
4% 2% 2% 0%
11% 18% 6%
65
6% 5% 2%
135 (100, 190) 9 (7, 17)
2%
6 (5, 8)
2% 5% 0% 2% 0% 5% 9% 2%
p
0.18 0.22 0.65 0.17 0.37 1.00 0.003 0.49 0.67 1.00 1.00 1.00 0.51 0.65 0.62
0.006 0.041 0.095 0.033 0.29 0.37 0.011 1.00 1.00 0.50 1.00 1.00 0.30 0.29 1.00
AKI: acute kidney injury; RIFLE: Risk, Injury, Failure, Loss of renal function and End-stage renal disease.
Categorical data are represented as %; continuous data as median (interquartile range). Combined morbidity; incidence of postoperative ventilation>48hours, new renal insufficiency, stroke or return to theatre.
DO2i on AKI has received recent attention.16 Although there was no difference between patients accepting and refusing transfusion overall in respect of DO2i, this study reveals a significant shift in DO2i in both groups from a level below the 270 threshold for greater renal impair- ment prior to 2013 to above this threshold in the 6years to 2019. Notably this shift was not due to a significant increase in CPB flow rate but likely attributed to the sig- nificant increase in minimum Hb over the two time peri- ods in both groups. Interestingly, while there were obvious increased blood conservation modalities employed in the
JW cohort, there was no perfusion management differ- ence between patients accepting and refusing transfusion overall in respect of DO2i. The precise relationship between DO2 and oxygen-derived parameters during CPB and AKI first became widely apparent compara- tively recently.19 Similarly, the recent more widespread availability of real-time non-invasive monitoring of derived oxygen parameters now provides the ability to use a so-called goal-directed perfusion to better match perfusion during CPB to individual patient physiological requirements.20
39 APRIL 2022 | www.anzcp.org