Page 5 - Test1
P. 5
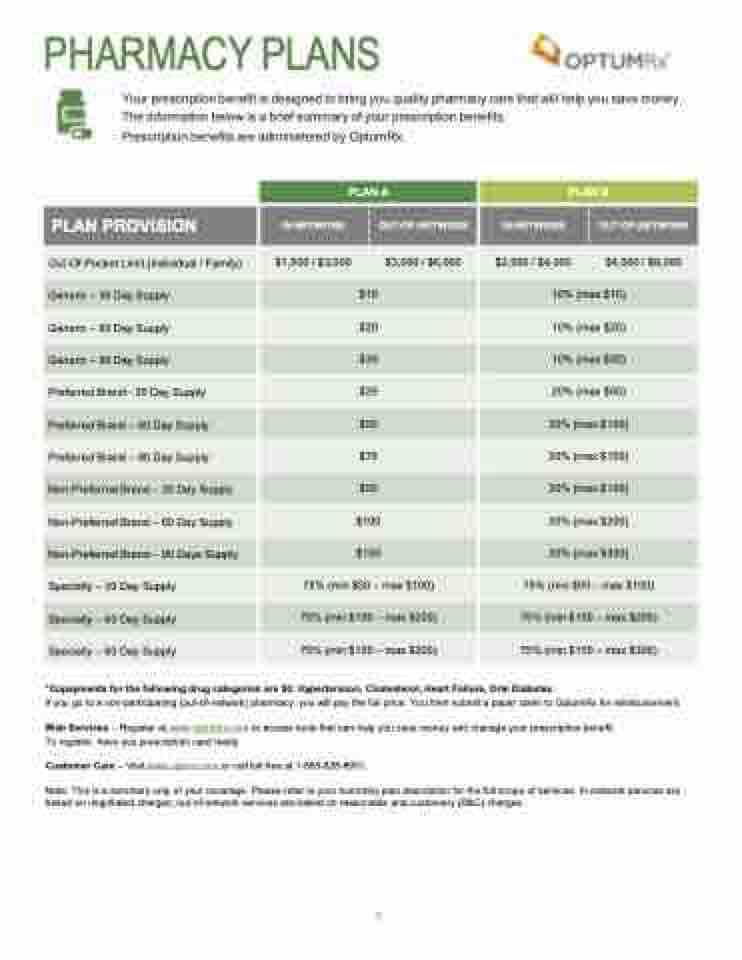
PHARMACY PLANS
Your prescription benefit is designed to bring you quality pharmacy care that will help you save money. The information below is a brief summary of your prescription benefits.
Prescription benefits are administered by OptumRx.
PLAN PROVISION
Out-Of-Pocket Limit (Individual / Family)
Generic – 30 Day Supply
Generic – 60 Day Supply
Generic – 90 Day Supply
Preferred Brand– 30 Day Supply
Preferred Brand – 60 Day Supply
Preferred Brand – 90 Day Supply
Non-Preferred Brand – 30 Day Supply
Non-Preferred Brand – 60 Day Supply
Non-Preferred Brand – 90 Days Supply
Specialty – 30 Day Supply
Specialty – 60 Day Supply
Specialty – 90 Day Supply
IN-NETWORK
$1,500 / $3,000
PLAN A
$10
$20
$30
$25
$50
$75
$50
$100
$150
75% (min $50 – max $100)
75% (min $100 – max $200)
75% (min $150 – max $300)
OUT-OF-NETWORK
$3,000 / $6,000
IN-NETWORK
$2,000 / $4,000
PLAN B
10% (max $10)
10% (max $20)
10% (max $30)
20% (max $50)
20% (max $100)
20% (max $150)
30% (max $100)
30% (max $200)
30% (max $300)
75% (min $50 – max $100)
75% (min $100 – max $200)
75% (min $150 – max $300)
OUT-OF-NETWORK
$4,000 / $8,000
*Copayments for the following drug categories are $0: Hypertension, Cholesterol, Heart Failure, Oral Diabetes.
If you go to a non-participating (out-of-network) pharmacy, you will pay the full price. You then submit a paper claim to OptumRx for reimbursement.
Web Services – Register at www.optumrx.com to access tools that can help you save money and manage your prescription benefit. To register, have you prescription card ready.
Customer Care – Visit www.optum.com or call toll free at 1-885-828-8951.
Note: This is a summary only of your coverage. Please refer to your summary plan description for the full scope of services. In-network services are
based on negotiated charges; out-of-network services are based on reasonable and customary (R&C) charges.
5