Page 26 - Upstream Rehabilitation
P. 26
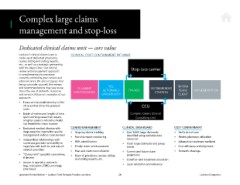
Complex large claims
management and stop-loss
Dedicated clinical claims unit — core value
Lockton’s clinical claims team is CLINICAL COST CONTAINMENT PATHWAY
made up of dedicated physicians,
nurses, billing and coding experts,
etc., as well as a strategic partnership
with the Mayo Clinic. Our clinical
review and management approach Stop-loss carrier
is complementary to processes
currently utilized by your carriers and
administrators. We also recognize that
being a provider yourself, the reviews
and recommendations may vary as we CLAIMANT YES, RECOMMENDED INFORM
stress the use of domestic resources IDENTIFICATION ACTIONABLE TPA/ASO STRATEGY TEAM/ IMPLEMENTATION
and services. Below are examples of our OPPORTUNITY CLIENT
approach:
• Focus on the small minority (<1%)
of cases that drive the greatest CCU
costs
• Depth of review and length of time Complex Claims Clinical
spent working cases that require Consulting Unit
a highly resource-intensive model
not feasible for many insurers
• Dedicated medical director with CLAIMS MANAGEMENT CLINICAL DASHBOARD COST CONTAINMENT
deep expertise in provider quality • Ongoing claims tracking • Over 9,000 large claimants • Verify site of care
management and cost containment • Monthly report monitoring identiied using available data • Review pharmacy utilization
• Independent relationships with resources
numerous providers and ability to • 85% identiication • Track large claimants and group • Alternative treatment methods
negotiate with both in- and out-of- • Timely claim reimbursement trends • Cost eficiency and alignment
network providers • Year-end claim reconciliation • Current and future claim • Domestic steerage
• “Concurrent” specialty case review, • Team of physicians, nurses, billing projections
if desired and coding experts, etc. • Condition and treatment education
• Access to specialty contracts
(e.g., transplant, ESRD, oncology, • Laser validation and reference
pharmacy)
Upstream Rehabilitation — Lockton Total Rewards Practice overview 26 Lockton Companies
management and stop-loss
Dedicated clinical claims unit — core value
Lockton’s clinical claims team is CLINICAL COST CONTAINMENT PATHWAY
made up of dedicated physicians,
nurses, billing and coding experts,
etc., as well as a strategic partnership
with the Mayo Clinic. Our clinical
review and management approach Stop-loss carrier
is complementary to processes
currently utilized by your carriers and
administrators. We also recognize that
being a provider yourself, the reviews
and recommendations may vary as we CLAIMANT YES, RECOMMENDED INFORM
stress the use of domestic resources IDENTIFICATION ACTIONABLE TPA/ASO STRATEGY TEAM/ IMPLEMENTATION
and services. Below are examples of our OPPORTUNITY CLIENT
approach:
• Focus on the small minority (<1%)
of cases that drive the greatest CCU
costs
• Depth of review and length of time Complex Claims Clinical
spent working cases that require Consulting Unit
a highly resource-intensive model
not feasible for many insurers
• Dedicated medical director with CLAIMS MANAGEMENT CLINICAL DASHBOARD COST CONTAINMENT
deep expertise in provider quality • Ongoing claims tracking • Over 9,000 large claimants • Verify site of care
management and cost containment • Monthly report monitoring identiied using available data • Review pharmacy utilization
• Independent relationships with resources
numerous providers and ability to • 85% identiication • Track large claimants and group • Alternative treatment methods
negotiate with both in- and out-of- • Timely claim reimbursement trends • Cost eficiency and alignment
network providers • Year-end claim reconciliation • Current and future claim • Domestic steerage
• “Concurrent” specialty case review, • Team of physicians, nurses, billing projections
if desired and coding experts, etc. • Condition and treatment education
• Access to specialty contracts
(e.g., transplant, ESRD, oncology, • Laser validation and reference
pharmacy)
Upstream Rehabilitation — Lockton Total Rewards Practice overview 26 Lockton Companies