Page 17 - Vidant Health
P. 17
Infolock
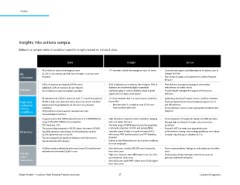
Insights into actions sample
Below is a sample table of condition-speciic insights based on Infolock data.
Data Insight Action
• $4.5 million in claims at emergency room • 227 members visited the emergency room 3+ times • Communicate urgent care/telemedicine to redirect care to
ER • 42.3% of visits were potentially non-emergent or primary care cheaper facilities
utilization treatable • Plan design changes can be punitive to address frequent
ER users
• 9.4% of members are diabetics (5.8% norm) • 82% of diabetics are moderate risk or higher; 74% of • Pilot diabetes management program and monitor
• Additional 3.6% of members are pre-diabetic diabetics are moderately/highly impactable effectiveness for wider rollout
Diabetes • $17.6 million in claims for diabetic members • Signiicant gaps in care for diabetics leads to great • Provide weight management support with access to
opportunity to impact claim spend dietitians
• 89 members had >$50K in claims for both 12-month time periods • 10.1% of members had 3 or more chronic conditions • Addressing obesity will impact chronic condition members
High-cost • 90.4% of high-cost claimants had at least one chronic condition (norm 8%) • Evaluate hypertension/musculoskeletal programs for it
claimants/ • Hypertension/hyperlipidemia are the two most prevalent − Members with 3+ conditions cost 12.9× more and effectiveness
chronic conditions than members with none • Second opinion services ensure appropriate treatment and
conditions • $38.8 million in claims were for members who had diagnosis
musculoskeletal condition
• Drug plan paid is $93 PMPM, below the norm of $100 PMPM; the • High utilization of generics when available is keeping • Promote generics through plan design and DAW penalties
range is $76-$151 PMPM across properties plan cost below the norm • Manage high-cost brands through custom formulary
• YOY trend was 11% • The wide range of PMPM spend across the properties exclusions
• The generic dispensing rate is 86.5%, above the norm of 84.6% is primarily a function of HCCs and varying PBMs • Review Rx HCCs to make sure appropriate prior
Pharmacy • Specialty spend as a percentage of total pharmacy spend is • Specialty spend is high as a result of several HCCs authorizations, dosing, and oncology guidelines are in place
54.2%, above the norm of 45.5% with cancer, PAH (cardiovascular), and ITP (bleeding • Consider step therapy on diabetes GLP-1s
• Top two categories by spend are diabetes and inlammatory disorder)
• Opioid utilization #5 category • Diabetes and inlammatory are the top two conditions
for most employers
• 4,769 procedures administered in most recent 12-month period • Non-clinic users used the ER 59% more frequently • Focus communication strategy on redirecting care to within
redirected an estimated $556K in care than clinic users clinic
On-site • High-cost claimants were 48% lower in cost for clinic • Evaluate plan design steerage, incentive structure to
clinic users than non-clinic users generate additional utilization
evaluation • Non-clinic users paid PMPY claims were 55.6% higher
than clinic users
Vidant Health — Lockton Total Rewards Practice overview 17 Lockton Companies
Insights into actions sample
Below is a sample table of condition-speciic insights based on Infolock data.
Data Insight Action
• $4.5 million in claims at emergency room • 227 members visited the emergency room 3+ times • Communicate urgent care/telemedicine to redirect care to
ER • 42.3% of visits were potentially non-emergent or primary care cheaper facilities
utilization treatable • Plan design changes can be punitive to address frequent
ER users
• 9.4% of members are diabetics (5.8% norm) • 82% of diabetics are moderate risk or higher; 74% of • Pilot diabetes management program and monitor
• Additional 3.6% of members are pre-diabetic diabetics are moderately/highly impactable effectiveness for wider rollout
Diabetes • $17.6 million in claims for diabetic members • Signiicant gaps in care for diabetics leads to great • Provide weight management support with access to
opportunity to impact claim spend dietitians
• 89 members had >$50K in claims for both 12-month time periods • 10.1% of members had 3 or more chronic conditions • Addressing obesity will impact chronic condition members
High-cost • 90.4% of high-cost claimants had at least one chronic condition (norm 8%) • Evaluate hypertension/musculoskeletal programs for it
claimants/ • Hypertension/hyperlipidemia are the two most prevalent − Members with 3+ conditions cost 12.9× more and effectiveness
chronic conditions than members with none • Second opinion services ensure appropriate treatment and
conditions • $38.8 million in claims were for members who had diagnosis
musculoskeletal condition
• Drug plan paid is $93 PMPM, below the norm of $100 PMPM; the • High utilization of generics when available is keeping • Promote generics through plan design and DAW penalties
range is $76-$151 PMPM across properties plan cost below the norm • Manage high-cost brands through custom formulary
• YOY trend was 11% • The wide range of PMPM spend across the properties exclusions
• The generic dispensing rate is 86.5%, above the norm of 84.6% is primarily a function of HCCs and varying PBMs • Review Rx HCCs to make sure appropriate prior
Pharmacy • Specialty spend as a percentage of total pharmacy spend is • Specialty spend is high as a result of several HCCs authorizations, dosing, and oncology guidelines are in place
54.2%, above the norm of 45.5% with cancer, PAH (cardiovascular), and ITP (bleeding • Consider step therapy on diabetes GLP-1s
• Top two categories by spend are diabetes and inlammatory disorder)
• Opioid utilization #5 category • Diabetes and inlammatory are the top two conditions
for most employers
• 4,769 procedures administered in most recent 12-month period • Non-clinic users used the ER 59% more frequently • Focus communication strategy on redirecting care to within
redirected an estimated $556K in care than clinic users clinic
On-site • High-cost claimants were 48% lower in cost for clinic • Evaluate plan design steerage, incentive structure to
clinic users than non-clinic users generate additional utilization
evaluation • Non-clinic users paid PMPY claims were 55.6% higher
than clinic users
Vidant Health — Lockton Total Rewards Practice overview 17 Lockton Companies