Page 86 - Down East Wood Ducks 2022 Benefits Guide
P. 86
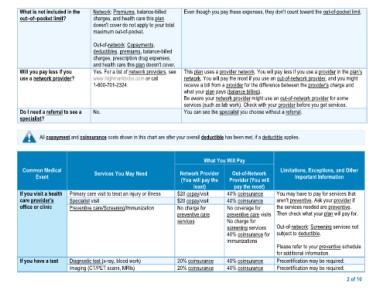
What is not included in the Network: Premiums, balance-billed Even though you pay these expenses, they don't count toward the out-of-pocket limit.
out–of–pocket limit?
charges, and health care this plan
Will you pay less if you doesn't cover do not apply to your total
use a network provider?
maximum out-of-pocket.
Do I need a referral to see a
specialist? Out-of-network: Copayments, This plan uses a provider network. You will pay less if you use a provider in the plan’s
deductibles, premiums, balance-billed network. You will pay the most if you use an out-of-network provider, and you might
charges, prescription drug expenses, receive a bill from a provider for the difference between the provider’s charge and
and health care this plan doesn't cover. what your plan pays (balance billing).
Yes. For a list of network providers, see Be aware your network provider might use an out-of-network provider for some
www.highmarkbcbs.com or call services (such as lab work). Check with your provider before you get services.
1-800-701-2324.
You can see the specialist you choose without a referral.
No.
All copayment and coinsurance costs shown in this chart are after your overall deductible has been met, if a deductible applies.
What You Will Pay
Common Medical Services You May Need Network Provider Out-of-Network Limitations, Exceptions, and Other
Event (You will pay the Provider (You will Important Information
If you visit a health Primary care visit to treat an injury or illness least) pay the most) You may have to pay for services that
care provider’s Specialist visit aren’t preventive. Ask your provider if
office or clinic Preventive care/Screening/Immunization $20 copay/visit 40% coinsurance the services needed are preventive.
Then check what your plan will pay for.
$20 copay/visit 40% coinsurance
Out-of-network: Screening services not
No charge for No coverage for subject to deductible.
preventive care preventive care visits
services No charge for Please refer to your preventive schedule
screening services for additional information.
40% coinsurance for Precertification may be required.
immunizations Precertification may be required.
If you have a test Diagnostic test (x-ray, blood work) 20% coinsurance 40% coinsurance
Imaging (CT/PET scans, MRIs) 20% coinsurance 40% coinsurance
2 of 10