Page 125 - Touching All the Bases- Power point 2023 v2_Neat
P. 125
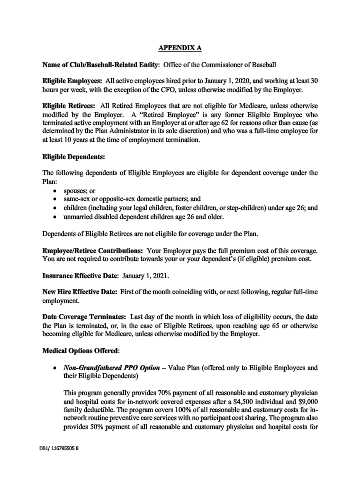
APPENDIX A
Name of Club/Baseball-Related Entity: Office of the Commissioner of Baseball
Eligible Employees: All active employees hired prior to January 1, 2020, and working at least 30
hours per week, with the exception of the CFO, unless otherwise modified by the Employer.
Eligible Retirees: All Retired Employees that are not eligible for Medicare, unless otherwise
modified by the Employer. A “Retired Employee” is any former Eligible Employee who
terminated active employment with an Employer at or after age 62 for reasons other than cause (as
determined by the Plan Administrator in its sole discretion) and who was a full-time employee for
at least 10 years at the time of employment termination.
Eligible Dependents:
The following dependents of Eligible Employees are eligible for dependent coverage under the
Plan:
• spouses; or
• same-sex or opposite-sex domestic partners; and
• children (including your legal children, foster children, or step-children) under age 26; and
• unmarried disabled dependent children age 26 and older.
Dependents of Eligible Retirees are not eligible for coverage under the Plan.
Employee/Retiree Contributions: Your Employer pays the full premium cost of this coverage.
You are not required to contribute towards your or your dependent’s (if eligible) premium cost.
Insurance Effective Date: January 1, 2021.
New Hire Effective Date: First of the month coinciding with, or next following, regular full-time
employment.
Date Coverage Terminates: Last day of the month in which loss of eligibility occurs, the date
the Plan is terminated, or, in the case of Eligible Retirees, upon reaching age 65 or otherwise
becoming eligible for Medicare, unless otherwise modified by the Employer.
Medical Options Offered:
• Non-Grandfathered PPO Option – Value Plan (offered only to Eligible Employees and
their Eligible Dependents)
This program generally provides 70% payment of all reasonable and customary physician
and hospital costs for in-network covered expenses after a $4,500 individual and $9,000
family deductible. The program covers 100% of all reasonable and customary costs for in-
network routine preventive care services with no participant cost sharing. The program also
provides 50% payment of all reasonable and customary physician and hospital costs for
DB1/ 116795505.8