Page 66 - Avatar 2022 Flipbook
P. 66
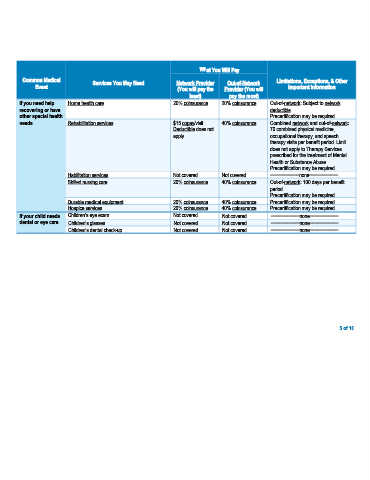
What You Will Pay
Common Medical Services You May Need Network Provider Out-of-Network Limitations, Exceptions, & Other
Event (You will pay the Provider (You will Important Information
least) pay the most)
If you need help Home health care 20% coinsurance 20% coinsurance Out-of-network: Subject to network
recovering or have deductible.
other special health Precertification may be required.
needs Rehabilitation services $15 copay/visit 40% coinsurance Combined network and out-of-network:
Deductible does not 70 combined physical medicine,
apply. occupational therapy, and speech
therapy visits per benefit period. Limit
does not apply to Therapy Services
prescribed for the treatment of Mental
Health or Substance Abuse.
Precertification may be required.
Habilitation services Not covered Not covered −−−−−−−−−−−none−−−−−−−−−−−
Skilled nursing care 20% coinsurance 40% coinsurance Out-of-network: 100 days per benefit
period.
Precertification may be required.
Durable medical equipment 20% coinsurance 40% coinsurance Precertification may be required.
Hospice services 20% coinsurance 40% coinsurance Precertification may be required.
If your child needs Children’s eye exam Not covered Not covered −−−−−−−−−−−none−−−−−−−−−−−
dental or eye care Children’s glasses Not covered Not covered −−−−−−−−−−−none−−−−−−−−−−−
Children’s dental check-up Not covered Not covered −−−−−−−−−−−none−−−−−−−−−−−
5 of 10