Page 5 - 03- Barrett Esophagus
P. 5
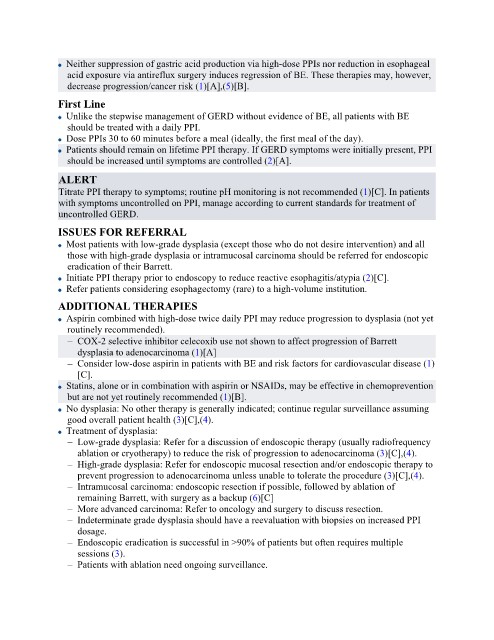
Neither suppression of gastric acid production via high-dose PPIs nor reduction in esophageal
acid exposure via antireflux surgery induces regression of BE. These therapies may, however,
decrease progression/cancer risk (1)[A],(5)[B].
First Line
Unlike the stepwise management of GERD without evidence of BE, all patients with BE
should be treated with a daily PPI.
Dose PPIs 30 to 60 minutes before a meal (ideally, the first meal of the day).
Patients should remain on lifetime PPI therapy. If GERD symptoms were initially present, PPI
should be increased until symptoms are controlled (2)[A].
ALERT
Titrate PPI therapy to symptoms; routine pH monitoring is not recommended (1)[C]. In patients
with symptoms uncontrolled on PPI, manage according to current standards for treatment of
uncontrolled GERD.
ISSUES FOR REFERRAL
Most patients with low-grade dysplasia (except those who do not desire intervention) and all
those with high-grade dysplasia or intramucosal carcinoma should be referred for endoscopic
eradication of their Barrett.
Initiate PPI therapy prior to endoscopy to reduce reactive esophagitis/atypia (2)[C].
Refer patients considering esophagectomy (rare) to a high-volume institution.
ADDITIONAL THERAPIES
Aspirin combined with high-dose twice daily PPI may reduce progression to dysplasia (not yet
routinely recommended).
– COX-2 selective inhibitor celecoxib use not shown to affect progression of Barrett
dysplasia to adenocarcinoma (1)[A]
– Consider low-dose aspirin in patients with BE and risk factors for cardiovascular disease (1)
[C].
Statins, alone or in combination with aspirin or NSAIDs, may be effective in chemoprevention
but are not yet routinely recommended (1)[B].
No dysplasia: No other therapy is generally indicated; continue regular surveillance assuming
good overall patient health (3)[C],(4).
Treatment of dysplasia:
– Low-grade dysplasia: Refer for a discussion of endoscopic therapy (usually radiofrequency
ablation or cryotherapy) to reduce the risk of progression to adenocarcinoma (3)[C],(4).
– High-grade dysplasia: Refer for endoscopic mucosal resection and/or endoscopic therapy to
prevent progression to adenocarcinoma unless unable to tolerate the procedure (3)[C],(4).
– Intramucosal carcinoma: endoscopic resection if possible, followed by ablation of
remaining Barrett, with surgery as a backup (6)[C]
– More advanced carcinoma: Refer to oncology and surgery to discuss resection.
– Indeterminate grade dysplasia should have a reevaluation with biopsies on increased PPI
dosage.
– Endoscopic eradication is successful in >90% of patients but often requires multiple
sessions (3).
– Patients with ablation need ongoing surveillance.