Page 4 - 02- Ascites (Cổ chướng)
P. 4
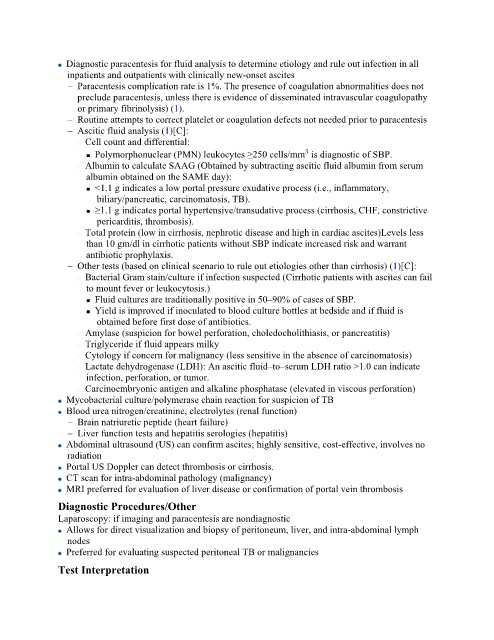
Diagnostic paracentesis for fluid analysis to determine etiology and rule out infection in all
inpatients and outpatients with clinically new-onset ascites
– Paracentesis complication rate is 1%. The presence of coagulation abnormalities does not
preclude paracentesis, unless there is evidence of disseminated intravascular coagulopathy
or primary fibrinolysis) (1).
– Routine attempts to correct platelet or coagulation defects not needed prior to paracentesis
– Ascitic fluid analysis (1)[C]:
Cell count and differential:
3
Polymorphonuclear (PMN) leukocytes ≥250 cells/mm is diagnostic of SBP.
Albumin to calculate SAAG (Obtained by subtracting ascitic fluid albumin from serum
albumin obtained on the SAME day):
<1.1 g indicates a low portal pressure exudative process (i.e., inflammatory,
biliary/pancreatic, carcinomatosis, TB).
≥1.1 g indicates portal hypertensive/transudative process (cirrhosis, CHF, constrictive
pericarditis, thrombosis).
Total protein (low in cirrhosis, nephrotic disease and high in cardiac ascites)Levels less
than 10 gm/dl in cirrhotic patients without SBP indicate increased risk and warrant
antibiotic prophylaxis.
– Other tests (based on clinical scenario to rule out etiologies other than cirrhosis) (1)[C]:
Bacterial Gram stain/culture if infection suspected (Cirrhotic patients with ascites can fail
to mount fever or leukocytosis.)
Fluid cultures are traditionally positive in 50–90% of cases of SBP.
Yield is improved if inoculated to blood culture bottles at bedside and if fluid is
obtained before first dose of antibiotics.
Amylase (suspicion for bowel perforation, choledocholithiasis, or pancreatitis)
Triglyceride if fluid appears milky
Cytology if concern for malignancy (less sensitive in the absence of carcinomatosis)
Lactate dehydrogenase (LDH): An ascitic fluid–to–serum LDH ratio >1.0 can indicate
infection, perforation, or tumor.
Carcinoembryonic antigen and alkaline phosphatase (elevated in viscous perforation)
Mycobacterial culture/polymerase chain reaction for suspicion of TB
Blood urea nitrogen/creatinine, electrolytes (renal function)
– Brain natriuretic peptide (heart failure)
– Liver function tests and hepatitis serologies (hepatitis)
Abdominal ultrasound (US) can confirm ascites; highly sensitive, cost-effective, involves no
radiation
Portal US Doppler can detect thrombosis or cirrhosis.
CT scan for intra-abdominal pathology (malignancy)
MRI preferred for evaluation of liver disease or confirmation of portal vein thrombosis
Diagnostic Procedures/Other
Laparoscopy: if imaging and paracentesis are nondiagnostic
Allows for direct visualization and biopsy of peritoneum, liver, and intra-abdominal lymph
nodes
Preferred for evaluating suspected peritoneal TB or malignancies
Test Interpretation