Page 37 - WNS 2022 E-Program Booklet
P. 37
The Impact of COVID-19 on Resident Training in Los Angeles County
Benjamin Yim, MD, John Muir Health
Co-authors: Michelle Lin, MD, University of Southern California, Elliot T. Min,
MD, University of Miami, Daniel Donoho MD, Children’s National Medical Cen-
ter at George Washington University, Steven L. Giannotta, MD, University of
Southern California
Introduction
In the aftermath of the COVID pandemic, assessment of its impact on resident
training following the emergent redistribution of staff and resources, particularly
in focal surge centers (i.e. New York City, Los Angeles), have not yet been
described.
Methods
Case logs of residents at the University of Southern California Department of
Neurological Surgery were reviewed from 7/1/2019 to 6/30/2021 while rotating
at LAC+USC, Keck Hospital, and Children’s Hospital Los Angeles (CHLA).
Procedure and resident involvement were compared between periods of
COVID-19 mandates (3/19/2020 to 5/4/2020 and 11/27/2020 to 1/25/2021) to
periods outside of these dates. Rates were calculated as cases logged/30 day
and cases logged/30 day/resident, compared to the rates required for gradua-
tion according to case minimums set forth by the Accreditation Council for
Graduate Medical Education in neurological surgery.
Results
Non-COVID periods averaged 415.7 logged cases/30 day (LAC 231.1, Keck
165.4, CHLA 19.3) compared to 277.5 logged cases/30 day (LAC 150.3, Keck
113.0, CHLA 20.7) with fewer assistant roles during periods of pandemic surg-
es. Spine cases were the most affected with a reduction of 46% (67 cases
logged/30 day) but nearly maintaining the rate to match the minimum require-
ments for ACGME graduation guidelines. Cerebrovascular (29.9 cases
logged/30 day during non-COVID vs. 24.1 cases logged/30 day), cranial tumor
(46.4 cases logged/30 days during non-COVID vs. 25.2 cases logged/30 day),
and cranial trauma case rates (40.6 cases logged/30 day during non-COVID
vs. 35.3 cases logged/30 days) remained well above the required case mini-
mums even during COVID restriction periods.
Conclusion
Despite reallocation of hospital resources to address the unprecedented de-
mands of the Covid-19 pandemic in the Los Angeles area, residents continued
to maintain a rate of total all defined case minimums (senior + lead only)/30
days at 53% higher than the ACGME minimum rate and for cerebrovascular,
cranial tumor, and cranial trauma case minimums.
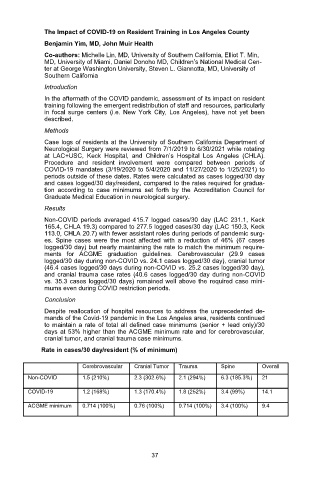
Rate in cases/30 day/resident (% of minimum)
Cerebrovascular Cranial Tumor Trauma Spine Overall
Non-COVID 1.5 (210%) 2.3 (302.6%) 2.1 (294%) 6.3 (185.3%) 21
COVID-19 1.2 (168%) 1.3 (170.4%) 1.8 (252%) 3.4 (99%) 14.1
ACGME minimum 0.714 (100%) 0.76 (100%) 0.714 (100%) 3.4 (100%) 9.4
37