Page 36 - C:\Users\jsalazar145\Documents\Flip PDF Professional\new-employees-benefits-guide-2019 030619\
P. 36
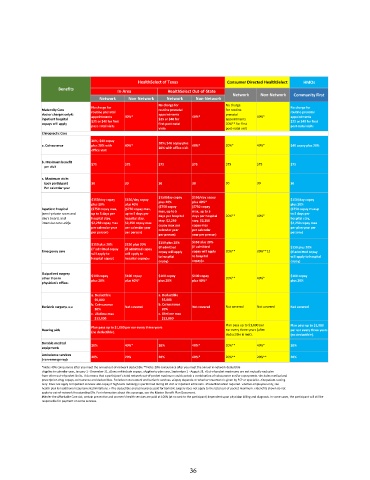
HealthSelect of Texas Consumer Directed HealthSelect HMOs
Benefits In-Area HealthSelect Out-of-State
Network Non-Network Community First
Network Non-Network Network Non-Network
No charge for No charge
No charge for No charge for
Maternity Care routine prenatal routine prenatal for routine routine prenatal
doctor charges only#; appointments 40%* appointments 40%* prenatal 40%* appointments
inpatient hospital $25 or $40 for first $25 or $40 for appointments $25 or $40 for first
copays will apply first post-natal 20%** for first
post-natal visit6 post-natal visit post-natal visit6
visit6
Chiropractic Care
20%; $40 copay
a. Coinsurance plus 20% with 40%* 20%; $40 copay plus 40%* 20%* 40%* $40 copay plus 20%
20% with office visit
office visit
b. Maximum benefit $75 $75
per visit $75 $75 $75 $75 $75
c. Maximum visits
Each participant 30 30 30 30 30 30 30
Per calendar year
$150/day copay $150/day copay
$150/day copay $150/day copay $150/day copay
plus 20% plus 40% plus 20% plus 40%* plus 20%
Inpatient hospital ($750 copay max, ($750 copay max, ($750 copay ($750 copay ($750 copay maxup
max, up to 5
max, up to 5
(semi-private room and up to 5 days per up to 5 days per days per hospital days per hospital 20%** 40%* to 5 days per
day’s board, and hospital stay. hospital stay. stay. $2,250 stay. $2,250 hospital stay,
intensive care unit)9 $2,250 copay max $2,250 copay max copay max per copay max $2,250 copay max
per calendar year per calendar year calendar year per calendar per plan year per
per person) per person) person3)
per person) year per person)
$150 plus 20% $150 plus 20% $150 plus 20% $150 plus 20%
(if admitted
(if admitted copay (if admitted copay (if admitted $150 plus 20%
Emergency care copay will apply copay will apply 20%** 20%**12 (if admitted copay
will apply to will apply to to hospital
hospital copay) hospital copay)12 to hospital will apply to hospital
copay) copay)12 copay)
Outpatient surgery
other than in $100 copay $100 copay $100 copay $100 copay 20%** 40%* $100 copay
plus 20% plus 40%* plus 20% plus 40%* plus 20%
physician’s office9
a. Deductible a. Deductible
$5,000 $5,000
b. Coinsurance b. Coinsurance
Bariatric surgery9,10,11 Not covered Not covered Not covered Not covered Not covered
20% 20%
c. Lifetime max c. Lifetime max
$13,000 $13,000
Plan pays up to $1,000 per Plan pays up to $1,000
Plan pays up to $1,000 per ear every three years
Hearing aids (no deductible). ear every three years (after per ear every three years
deductible is met). (no deductible).
Durable medical 20% 40%* 20% 40%* 20%** 40%* 20%
equipment9
Ambulance services
20% 20% 20% 40%* 20%** 20%** 20%
(non-emergency)9
*Note: 40% coinsurance after you meet the annual out-of-network deductible **Note: 20% coinsurance after you meet the annual in-network deductible
1Applies to calendar year, January 1 - December 31. 2Does not include copays. 3Applies to plan year, September 1 - August 31. 4Out-of-pocket maximums are not mutually exclusive
from other out-of-pocket limits. This means that a participant’s total network out-of-pocket maximum could contain a combination of coinsurance and/or copayments. 5Includes medical and
prescription drug copays, coinsurance and deductibles. Excludes non-network and bariatric services. 6Copay depends on whether treatment is given by PCP or specialist. 7Outpatient testing
only. Does not apply to inpatient services. 8No copay if high-tech radiology is performed during ER visit or inpatient admission. 9Preauthorization required. 10Active employees only; see
health plan for additional requirements/limitations. 11The deductible and coinsurance paid for bariatric surgery does not apply to the total out-of-pocket maximum. 12Benefits shown do not
apply to out-of-network freestanding ERs. For information about this coverage, see the Master Benefit Plan Document.
#Under the Affordable Care Act, certain preventive and women’s health services are paid at 100% (at no cost to the participant) dependent upon physician billing and diagnosis. In some cases, the participant will still be
responsible for payment on some services.
36