Page 3 - e-book QR - BIPOLAR DISORDER 2ND ED (pruf 3)
P. 3
QUICK REFERENCE MANAGEMENT OF BIPOLAR DISORDER (2ND EDITION)
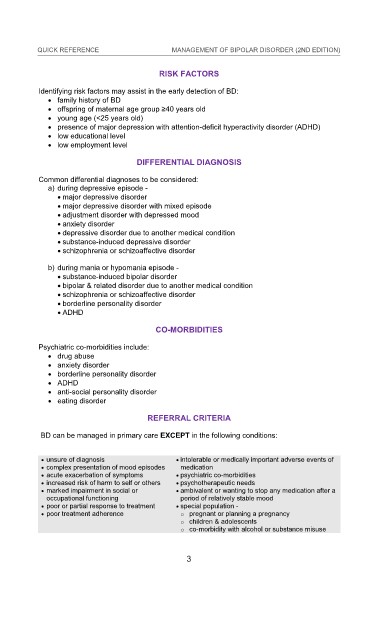
RISK FACTORS
KEY MESSAGES
Identifying risk factors may assist in the early detection of BD:
1. Bipolar Disorder (BD) is a potentially life-long con family history of BD
KEY MESSAGES dition presenting commonly as
either bipolar I disorder (BD I) or bipolar II disorder (BD II). BD I is characterised offspring of maternal age group ≥40 years old
1. Bipolar Disorder (BD) is a potentially life-long condition presenting commonly as young age (<25 years old) RISK FACTORS
by episodes of mania, whilst BD II is characterised by episodes of hypomania and
either bipolar I disorder (BD I) or bipolar II disorder (BD II). BD I is characterised
depressive episodes. presence of major depression with attention-deficit hyperactivity disorder (ADHD)
Identifying risk factors may assist in the early detection of BD:
low educational level
by episodes of mania, whilst BD II is characterised by episodes of hypomania and
2. BD should be diagnosed based on the Diagnostic and Statistical Manual of Mental low employment level
family history of BD
depressive episodes.
Disorders Fifth Edition, Text Revision (DSM-5-TR) or International Classification offspring of maternal age group ≥40 years old
2. BD should be diagnosed based on the Diagnostic and Statistical Manual of Mental young age (<25 years old)
DIFFERENTIAL DIAGNOSIS
of Diseases Eleventh Revision (ICD-11).
Disorders Fifth Edition, Text Revision (DSM-5-TR) or International Classification
3. Antipsychotics (APs) or mood stabilisers, either as monotherapy or combination, presence of major depression with attention-deficit hyperactivity disorder (ADHD)
low educational level
of Diseases Eleventh Revision (ICD-11).
low employment level
should be used to treat acute mood episodes (mania, depressive and mixed Common differential diagnoses to be considered:
3. Antipsychotics (APs) or mood stabilisers, either as monotherapy or combination, a) during depressive episode -
episodes) & as maintenance therapy in BD.
major depressive disorder
DIFFERENTIAL DIAGNOSIS
should be used to treat acute mood episodes (mania, depressive and mixed
4. For BD with anxious distress, AAPs may be used. major depressive disorder with mixed episode
episodes) & as maintenance therapy in BD.
adjustment disorder with depressed mood
5. For BD with rapid cycling, a combination of mood stabilisers with AAPs or another Common differential diagnoses to be considered:
4. For BD with anxious distress, AAPs may be used. anxiety disorder
a) during depressive episode -
mood stabiliser is the preferred treatment of choice.
major depressive disorder
5. For BD with rapid cycling, a combination of mood stabilisers with AAPs or another
6. Antidepressants (AD) may be used as short-term adjunctive treatment but not as depressive disorder due to another medical condition
major depressive disorder with mixed episode
substance-induced depressive disorder
mood stabiliser is the preferred treatment of choice.
adjustment disorder with depressed mood
monotherapy in BD. It should be avoided in mixed episodes & used with caution schizophrenia or schizoaffective disorder
6. Antidepressants (AD) may be used as short-term adjunctive treatment but not as anxiety disorder
in rapid cycling BD.
depressive disorder due to another medical condition
monotherapy in BD. It should be avoided in mixed episodes & used with caution
7. Long-acting AAP injectables may be considered in BD patients who have poor b) during mania or hypomania episode -
substance-induced depressive disorder
in rapid cycling BD.
adherence to oral medications. substance-induced bipolar disorder
schizophrenia or schizoaffective disorder
7. Long-acting AAP injectables may be considered in BD patients who have poor
8. Electroconvulsive therapy should be considered in both bipolar manic & bipolar & related disorder due to another medical condition
schizophrenia or schizoaffective disorder
b) during mania or hypomania episode -
adherence to oral medications.
depressive episodes in indicated situations (refer to Algorithm 1 & 2). borderline personality disorder
substance-induced bipolar disorder
8. Electroconvulsive therapy should be considered in both bipolar manic &
9. Psychosocial interventions & psychotherapies should be offered as an adjunctive ADHD
bipolar & related disorder due to another medical condition
depressive episodes in indicated situations (refer to Algorithm 1 & 2).
treatment for BD especially in relapse prevention. schizophrenia or schizoaffective disorder
CO-MORBIDITIES
9. Psychosocial interventions & psychotherapies should be offered as an adjunctive
10. Shared decision-making in weighing risks vs benefits of pharmacological borderline personality disorder
ADHD
treatment for BD especially in relapse prevention.
treatment should be done in pregnant & lactating women with BD. Psychiatric co-morbidities include:
10. Shared decision-making in weighing risks vs benefits of pharmacological drug abuse CO-MORBIDITIES
treatment should be done in pregnant & lactating women with BD. anxiety disorder
Psychiatric co-morbidities include:
This Quick Reference provides key messages & a summary of the main recommendations borderline personality disorder
drug abuse
in the Clinical Practice Guidelines (CPG) Management of Bipolar Disorder (Second Edition). ADHD
anxiety disorder
This Quick Reference provides key messages & a summary of the main recommendations anti-social personality disorder
borderline personality disorder
Details of the evidence supporting these recommendations can be found in the above
in the Clinical Practice Guidelines (CPG) Management of Bipolar Disorder (Second Edition). eating disorder
ADHD
CPG, available on the following websites: anti-social personality disorder
Details of the evidence supporting these recommendations can be found in the above eating disorder REFERRAL CRITERIA
Ministry of Health Malaysia: www.moh.gov.my
CPG, available on the following websites:
Academy of Medicine Malaysia: www.acadmed.org.my REFERRAL CRITERIA
Malaysian Psychiatric Association: www.psychiatry-malaysia.org BD can be managed in primary care EXCEPT in the following conditions:
Ministry of Health Malaysia: www.moh.gov.my
BD can be managed in primary care EXCEPT in the following conditions:
Academy of Medicine Malaysia: www.acadmed.org.my unsure of diagnosis intolerable or medically important adverse events of
medication
Malaysian Psychiatric Association: www.psychiatry-malaysia.org complex presentation of mood episodes intolerable or medically important adverse events of
CLINICAL PRACTICE GUIDELINES SECRETARIAT
unsure of diagnosis
Malaysian Health Technology Assessment Section (MaHTAS) acute exacerbation of symptoms psychiatric co-morbidities
medication
complex presentation of mood episodes
Medical Development Division, Ministry of Health Malaysia increased risk of harm to self or others psychotherapeutic needs
psychiatric co-morbidities
acute exacerbation of symptoms
CLINICAL PRACTICE GUIDELINES SECRETARIAT
increased risk of harm to self or others
psychotherapeutic needs
Level 4, Block E1, Precinct 1
Malaysian Health Technology Assessment Section (MaHTAS) marked impairment in social or ambivalent or wanting to stop any medication after a
period of relatively stable mood
occupational functioning
ambivalent or wanting to stop any medication after a
marked impairment in social or
Federal Government Administrative Centre 62590
Medical Development Division, Ministry of Health Malaysia
period of relatively stable mood
occupational functioning
Putrajaya, Malaysia
Level 4, Block E1, Precinct 1 poor or partial response to treatment special population -
poor or partial response to treatment
o pregnant or planning a pregnancy
Tel: 603-88831229
Federal Government Administrative Centre 62590 poor treatment adherence special population -
poor treatment adherence
o pregnant or planning a pregnancy
E-mail: htamalaysia@moh.gov.my o children & adolescents
Putrajaya, Malaysia
o children & adolescents
Tel: 603-88831229 o co-morbidity with alcohol or substance misuse
o co-morbidity with alcohol or substance misuse
E-mail: htamalaysia@moh.gov.my
3
2 3
2 3
2
QR - BIPOLAR DISORDER 2ND ED.indd 3 12/24/2024 2:40:58 PM