Page 39 - Risk Reduction Series - Documentation Essentials (Part One)
P. 39
SVMIC Risk Reduction Series: Documentation Essentials
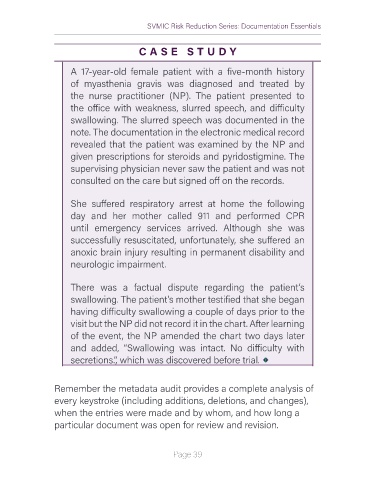
C A S E S T U DY
A 17-year-old female patient with a five-month history
of myasthenia gravis was diagnosed and treated by
the nurse practitioner (NP). The patient presented to
the office with weakness, slurred speech, and difficulty
swallowing. The slurred speech was documented in the
note. The documentation in the electronic medical record
revealed that the patient was examined by the NP and
given prescriptions for steroids and pyridostigmine. The
supervising physician never saw the patient and was not
consulted on the care but signed off on the records.
She suffered respiratory arrest at home the following
day and her mother called 911 and performed CPR
until emergency services arrived. Although she was
successfully resuscitated, unfortunately, she suffered an
anoxic brain injury resulting in permanent disability and
neurologic impairment.
There was a factual dispute regarding the patient’s
swallowing. The patient’s mother testified that she began
having difficulty swallowing a couple of days prior to the
visit but the NP did not record it in the chart. After learning
of the event, the NP amended the chart two days later
and added, “Swallowing was intact. No difficulty with
secretions.”, which was discovered before trial.
Remember the metadata audit provides a complete analysis of
every keystroke (including additions, deletions, and changes),
when the entries were made and by whom, and how long a
particular document was open for review and revision.
Page 39