Page 15 - QCS.19 SPD - PPO
P. 15
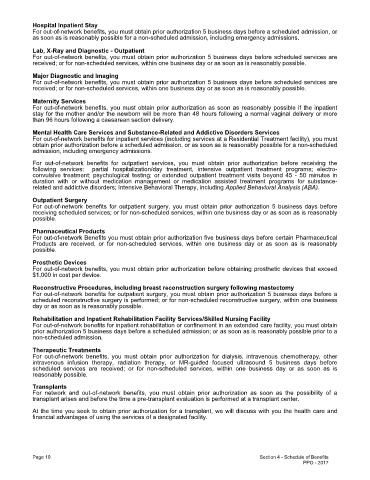
Hospital Inpatient Stay
For out-of-network benefits, you must obtain prior authorization 5 business days before a scheduled admission, or
as soon as is reasonably possible for a non-scheduled admission, including emergency admissions.
Lab, X-Ray and Diagnostic - Outpatient
For out-of-network benefits, you must obtain prior authorization 5 business days before scheduled services are
received; or for non-scheduled services, within one business day or as soon as is reasonably possible.
Major Diagnostic and Imaging
For out-of-network benefits, you must obtain prior authorization 5 business days before scheduled services are
received; or for non-scheduled services, within one business day or as soon as is reasonably possible.
Maternity Services
For out-of-network benefits, you must obtain prior authorization as soon as reasonably possible if the inpatient
stay for the mother and/or the newborn will be more than 48 hours following a normal vaginal delivery or more
than 96 hours following a caesarean section delivery.
Mental Health Care Services and Substance-Related and Addictive Disorders Services
For out-of-network benefits for inpatient services (including services at a Residential Treatment facility), you must
obtain prior authorization before a scheduled admission, or as soon as is reasonably possible for a non-scheduled
admission, including emergency admissions.
For out-of-network benefits for outpatient services, you must obtain prior authorization before receiving the
following services: partial hospitalization/day treatment, intensive outpatient treatment programs; electro-
convulsive treatment; psychological testing; or extended outpatient treatment visits beyond 45 - 50 minutes in
duration with or without medication management or medication assisted treatment programs for substance-
related and addictive disorders; Intensive Behavioral Therapy, including Applied Behavioral Analysis (ABA).
Outpatient Surgery
For out-of-network benefits for outpatient surgery, you must obtain prior authorization 5 business days before
receiving scheduled services; or for non-scheduled services, within one business day or as soon as is reasonably
possible.
Pharmaceutical Products
For out-of-network Benefits you must obtain prior authorization five business days before certain Pharmaceutical
Products are received, or for non-scheduled services, within one business day or as soon as is reasonably
possible.
Prosthetic Devices
For out-of-network benefits, you must obtain prior authorization before obtaining prosthetic devices that exceed
$1,000 in cost per device.
Reconstructive Procedures, including breast reconstruction surgery following mastectomy
For out-of-network benefits for outpatient surgery, you must obtain prior authorization 5 business days before a
scheduled reconstructive surgery is performed; or for non-scheduled reconstructive surgery, within one business
day or as soon as is reasonably possible.
Rehabilitation and Inpatient Rehabilitation Facility Services/Skilled Nursing Facility
For out-of-network benefits for inpatient rehabilitation or confinement in an extended care facility, you must obtain
prior authorization 5 business days before a scheduled admission; or as soon as is reasonably possible prior to a
non-scheduled admission.
Therapeutic Treatments
For out-of-network benefits, you must obtain prior authorization for dialysis, intravenous chemotherapy, other
intravenous infusion therapy, radiation therapy, or MR-guided focused ultrasound 5 business days before
scheduled services are received; or for non-scheduled services, within one business day or as soon as is
reasonably possible.
Transplants
For network and out-of-network benefits, you must obtain prior authorization as soon as the possibility of a
transplant arises and before the time a pre-transplant evaluation is performed at a transplant center.
At the time you seek to obtain prior authorization for a transplant, we will discuss with you the health care and
financial advantages of using the services of a designated facility.
Page 10 Section 4 - Schedule of Benefits
PPO - 2017