Page 57 - QCS.19 SPD - PPO
P. 57
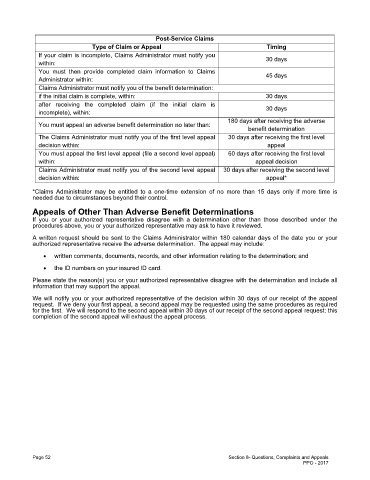
Post-Service Claims
Type of Claim or Appeal Timing
If your claim is incomplete, Claims Administrator must notify you
30 days
within:
You must then provide completed claim information to Claims
45 days
Administrator within:
Claims Administrator must notify you of the benefit determination:
if the initial claim is complete, within: 30 days
after receiving the completed claim (if the initial claim is
30 days
incomplete), within:
180 days after receiving the adverse
You must appeal an adverse benefit determination no later than:
benefit determination
The Claims Administrator must notify you of the first level appeal 30 days after receiving the first level
decision within: appeal
You must appeal the first level appeal (file a second level appeal) 60 days after receiving the first level
within: appeal decision
Claims Administrator must notify you of the second level appeal 30 days after receiving the second level
decision within: appeal*
*Claims Administrator may be entitled to a one-time extension of no more than 15 days only if more time is
needed due to circumstances beyond their control.
Appeals of Other Than Adverse Benefit Determinations
If you or your authorized representative disagree with a determination other than those described under the
procedures above, you or your authorized representative may ask to have it reviewed.
A written request should be sent to the Claims Administrator within 180 calendar days of the date you or your
authorized representative receive the adverse determination. The appeal may include:
· written comments, documents, records, and other information relating to the determination; and
· the ID numbers on your insured ID card.
Please state the reason(s) you or your authorized representative disagree with the determination and include all
information that may support the appeal.
We will notify you or your authorized representative of the decision within 30 days of our receipt of the appeal
request. If we deny your first appeal, a second appeal may be requested using the same procedures as required
for the first. We will respond to the second appeal within 30 days of our receipt of the second appeal request; this
completion of the second appeal will exhaust the appeal process.
Page 52 Section 8- Questions, Complaints and Appeals
PPO - 2017