Page 7 - e-CPG-SLE-8_5_24
P. 7
Management of Systemic Lupus Erythematosus
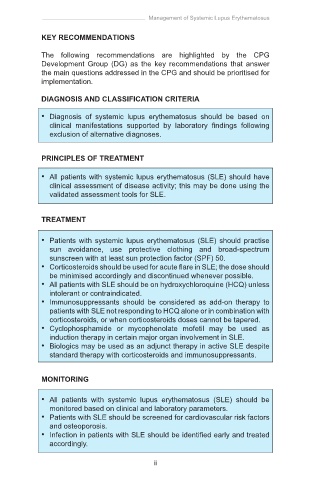
KEY RECOMMENDATIONS
The following recommendations are highlighted by the CPG
Development Group (DG) as the key recommendations that answer
the main questions addressed in the CPG and should be prioritised for
implementation.
DIAGNOSIS AND CLASSIFICATION CRITERIA
• Diagnosis of systemic lupus erythematosus should be based on
clinical manifestations supported by laboratory findings following
exclusion of alternative diagnoses.
PRINCIPLES OF TREATMENT
• All patients with systemic lupus erythematosus (SLE) should have
clinical assessment of disease activity; this may be done using the
validated assessment tools for SLE.
TREATMENT
• Patients with systemic lupus erythematosus (SLE) should practise
sun avoidance, use protective clothing and broad-spectrum
sunscreen with at least sun protection factor (SPF) 50.
• Corticosteroids should be used for acute flare in SLE; the dose should
be minimised accordingly and discontinued whenever possible.
• All patients with SLE should be on hydroxychloroquine (HCQ) unless
intolerant or contraindicated.
• Immunosuppressants should be considered as add-on therapy to
patients with SLE not responding to HCQ alone or in combination with
corticosteroids, or when corticosteroids doses cannot be tapered.
• Cyclophosphamide or mycophenolate mofetil may be used as
induction therapy in certain major organ involvement in SLE.
• Biologics may be used as an adjunct therapy in active SLE despite
standard therapy with corticosteroids and immunosuppressants.
MONITORING
• All patients with systemic lupus erythematosus (SLE) should be
monitored based on clinical and laboratory parameters.
• Patients with SLE should be screened for cardiovascular risk factors
and osteoporosis.
• Infection in patients with SLE should be identified early and treated
accordingly.
ii