Page 217 - MHF-FeedingMinds-final.indd
P. 217
208 7.3 Nutrition for Children with Chronic Diseases and Syndromes
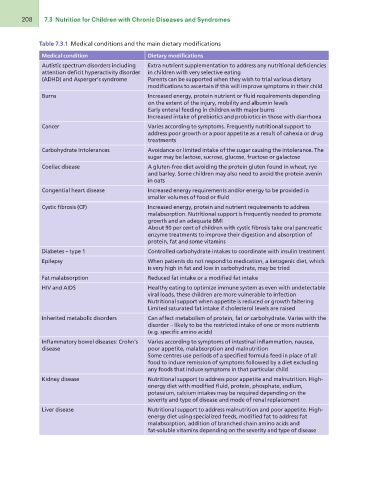
Table 7.3.1 Medical conditions and the main dietary modifications
Medical condition Dietary modifications
Autistic spectrum disorders including
attention deficit hyperactivity disorder Extra nutrient supplementation to address any nutritional deficiencies
(ADHD) and Asperger’s syndrome in children with very selective eating
Burns Parents can be supported when they wish to trial various dietary
modifications to ascertain if this will improve symptoms in their child
Cancer
Increased energy, protein nutrient or fluid requirements depending
Carbohydrate intolerances on the extent of the injury, mobility and albumin levels
Coeliac disease Early enteral feeding in children with major burns
Increased intake of prebiotics and probiotics in those with diarrhoea
Congential heart disease
Cystic fibrosis (CF) Varies according to symptoms. Frequently nutritional support to
address poor growth or a poor appetite as a result of cahexia or drug
Diabetes – type 1 treatments
Epilepsy
Fat malabsorption Avoidance or limited intake of the sugar causing the intolerance. The
HIV and AIDS sugar may be lactose, sucrose, glucose, fructose or galactose
Inherited metabolic disorders A gluten-free diet avoiding the protein gluten found in wheat, rye
and barley. Some children may also need to avoid the protein avenin
Inflammatory bowel diseases: Crohn’s in oats
disease
Increased energy requirements and/or energy to be provided in
Kidney disease smaller volumes of food or fluid
Liver disease Increased energy, protein and nutrient requirements to address
malabsorption. Nutritional support is frequently needed to promote
growth and an adequate BMI
About 90 per cent of children with cystic fibrosis take oral pancreatic
enzyme treatments to improve their digestion and absorption of
protein, fat and some vitamins
Controlled carbohydrate intakes to coordinate with insulin treatment
When patients do not respond to medication, a ketogenic diet, which
is very high in fat and low in carbohydrate, may be tried
Reduced fat intake or a modified fat intake
Healthy eating to optimize immune system as even with undetectable
viral loads, these children are more vulnerable to infection
Nutritional support when appetite is reduced or growth faltering
Limited saturated fat intake if cholesterol levels are raised
Can affect metabolism of protein, fat or carbohydrate. Varies with the
disorder – likely to be the restricted intake of one or more nutrients
(e.g. specific amino acids)
Varies according to symptoms of intestinal inflammation, nausea,
poor appetite, malabsorption and malnutrition
Some centres use periods of a specified formula feed in place of all
food to induce remission of symptoms followed by a diet excluding
any foods that induce symptoms in that particular child
Nutritional support to address poor appetite and malnutrition. High-
energy diet with modified fluid, protein, phosphate, sodium,
potassium, calcium intakes may be required depending on the
severity and type of disease and mode of renal replacement
Nutritional support to address malnutrition and poor appetite. High-
energy diet using specialized feeds, modified fat to address fat
malabsorption, addition of branched chain amino acids and
fat-soluble vitamins depending on the severity and type of disease