Page 144 - 2021 Medical Plan SPD
P. 144
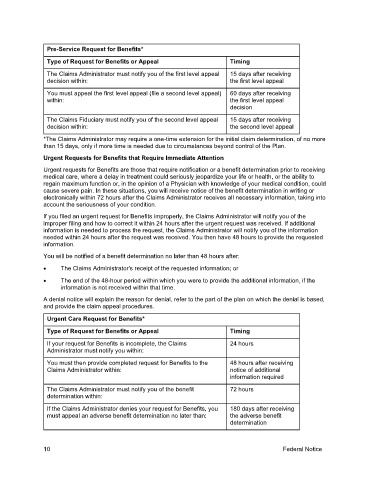
Pre-Service Request for Benefits*
Type of Request for Benefits or Appeal Timing
The Claims Administrator must notify you of the first level appeal 15 days after receiving
decision within: the first level appeal
You must appeal the first level appeal (file a second level appeal) 60 days after receiving
within: the first level appeal
decision
The Claims Fiduciary must notify you of the second level appeal 15 days after receiving
decision within: the second level appeal
*The Claims Administrator may require a one-time extension for the initial claim determination, of no more
than 15 days, only if more time is needed due to circumstances beyond control of the Plan.
Urgent Requests for Benefits that Require Immediate Attention
Urgent requests for Benefits are those that require notification or a benefit determination prior to receiving
medical care, where a delay in treatment could seriously jeopardize your life or health, or the ability to
regain maximum function or, in the opinion of a Physician with knowledge of your medical condition, could
cause severe pain. In these situations, you will receive notice of the benefit determination in writing or
electronically within 72 hours after the Claims Administrator receives all necessary information, taking into
account the seriousness of your condition.
If you filed an urgent request for Benefits improperly, the Claims Administrator will notify you of the
improper filing and how to correct it within 24 hours after the urgent request was received. If additional
information is needed to process the request, the Claims Administrator will notify you of the information
needed within 24 hours after the request was received. You then have 48 hours to provide the requested
information.
You will be notified of a benefit determination no later than 48 hours after:
• The Claims Administrator's receipt of the requested information; or
• The end of the 48-hour period within which you were to provide the additional information, if the
information is not received within that time.
A denial notice will explain the reason for denial, refer to the part of the plan on which the denial is based,
and provide the claim appeal procedures.
Urgent Care Request for Benefits*
Type of Request for Benefits or Appeal Timing
If your request for Benefits is incomplete, the Claims 24 hours
Administrator must notify you within:
You must then provide completed request for Benefits to the 48 hours after receiving
Claims Administrator within: notice of additional
information required
The Claims Administrator must notify you of the benefit 72 hours
determination within:
If the Claims Administrator denies your request for Benefits, you 180 days after receiving
must appeal an adverse benefit determination no later than: the adverse benefit
determination
10 Federal Notice