Page 30 - 2023 Employee Benefits Guide
P. 30
5. A determination by the Social Security Administration that a qualified
beneficiary is no longer disabled; beneficiary must notify us within 30
days after the later of 1) the date of final determination by the Social
Security Administration that the beneficiary is no longer disabled, or 2)
the date provided in the SPD or initial COBRA notice.
The above notices may be provided by the covered employee, a qualified
beneficiary with respect to the qualifying event, or a representative of
the employee or beneficiary. Notice by one individual will satisfy the
notice responsibility of all related qualifying beneficiaries with respect to
the qualifying event
If the employee or qualified beneficiary does not provide notice of the
events within the time limit provided above (with respect to each event),
Texas Mutual Insurance Company is not required to make COBRA
coverage available.
Proper notification by a current employee would be the employee
completing a benefit change in Workday or via a written notice. Proper
notification by a qualified beneficiary would be by written notice. The
written notice must include the name of the employee and qualifying
beneficiaries, the applicable qualifying event from the list above, the date
the qualifying event occurred, and the employee’s or qualifying
beneficiaries’ contact information. If notice is made in writing, it must be
either hand-delivered or mailed by United States mail, postage pre-paid,
and addressed to:
Attn: Human Resources—Employee Benefits
2200 Aldrich Street
Austin, TX 78723
COBRA coverage
If you elect to continue coverage under the Consolidated Omnibus
Budget Reconciliation Act of 1985 (COBRA), you and/or your dependents
will receive the same medical and dental benefits you were entitled to as
an employee provided you pay the COBRA premium. Qualifying events
for COBRA eligibility are listed in the chart below.
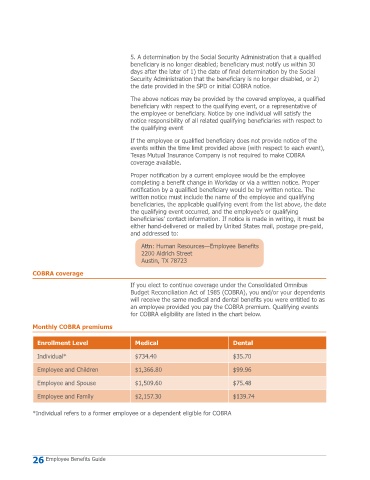
Monthly COBRA premiums
Enrollment Level Medical Dental
Individual* $734.40 $35.70
Employee and Children $1,366.80 $99.96
Employee and Spouse $1,509.60 $75.48
Employee and Family $2,157.30 $139.74
*Individual refers to a former employee or a dependent eligible for COBRA
26 Employee Benefits Guide