Page 154 - IC38 GENERAL INSURANCE
P. 154
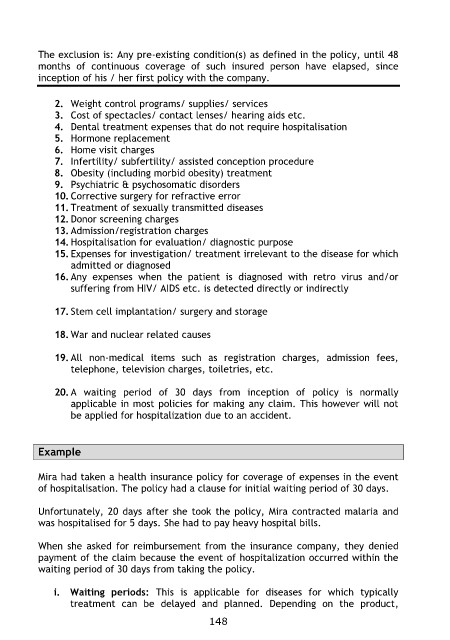
The exclusion is: Any pre-existing condition(s) as defined in the policy, until 48
months of continuous coverage of such insured person have elapsed, since
inception of his / her first policy with the company.
2. Weight control programs/ supplies/ services
3. Cost of spectacles/ contact lenses/ hearing aids etc.
4. Dental treatment expenses that do not require hospitalisation
5. Hormone replacement
6. Home visit charges
7. Infertility/ subfertility/ assisted conception procedure
8. Obesity (including morbid obesity) treatment
9. Psychiatric & psychosomatic disorders
10. Corrective surgery for refractive error
11. Treatment of sexually transmitted diseases
12. Donor screening charges
13. Admission/registration charges
14. Hospitalisation for evaluation/ diagnostic purpose
15. Expenses for investigation/ treatment irrelevant to the disease for which
admitted or diagnosed
16. Any expenses when the patient is diagnosed with retro virus and/or
suffering from HIV/ AIDS etc. is detected directly or indirectly
17. Stem cell implantation/ surgery and storage
18. War and nuclear related causes
19. All non-medical items such as registration charges, admission fees,
telephone, television charges, toiletries, etc.
20. A waiting period of 30 days from inception of policy is normally
applicable in most policies for making any claim. This however will not
be applied for hospitalization due to an accident.
Example
Mira had taken a health insurance policy for coverage of expenses in the event
of hospitalisation. The policy had a clause for initial waiting period of 30 days.
Unfortunately, 20 days after she took the policy, Mira contracted malaria and
was hospitalised for 5 days. She had to pay heavy hospital bills.
When she asked for reimbursement from the insurance company, they denied
payment of the claim because the event of hospitalization occurred within the
waiting period of 30 days from taking the policy.
i. Waiting periods: This is applicable for diseases for which typically
treatment can be delayed and planned. Depending on the product,
148