Page 22 - Friendship Village
P. 22
Complex large claims
management and stop-loss
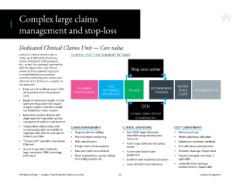
Dedicated Clinical Claims Unit — Core value
Lockton’s clinical claims team is CLINICAL COST CONTAINMENT PATHWAY
made up of dedicated physicians,
nurses, billing and coding experts,
etc., as well as a strategic partnership
with the Mayo Clinic. Our clinical
review and management approach Stop-loss carrier
is complementary to processes
currently utilized by your carriers and
administrators. Below are examples of
our approach: YES, INFORM
• Focus on the small minority (<1%) CLAIMANT ACTIONABLE TPA/ASO RECOMMENDED TEAM/ IMPLEMENTATION
of cases that drive the greatest IDENTIFICATION STRATEGY
costs OPPORTUNITY CLIENT
• Depth of review and length of time
spent working cases that require
a highly resource-intensive model CCU
not feasible for many insurers
• Dedicated medical director with Complex Claims Clinical
deep expertise in provider quality Consulting Unit
management and cost containment
• Independent relationships with CLAIMS MANAGEMENT CLINICAL DASHBOARD COST CONTAINMENT
numerous providers and ability to
negotiate with both in- and out-of- • Ongoing claims tracking • Over 9,000 large claimants • Verify site of care
network providers • Monthly report monitoring identiied using available data • Review pharmacy utilization
• “Concurrent” specialty case review, • 85% identiication resources • Alternative treatment methods
if desired • Timely claim reimbursement • Track large claimants and group • Cost eficiency and alignment
• Access to specialty contracts trends
(e.g., transplant, ESRD, oncology, • Year-end claim reconciliation • Current and future claim • Domestic steerage, if applicable
pharmacy) • Team of physicians, nurses, billing projections • Custom managed care rates, if
and coding experts, etc. • Condition and treatment education applicable
• Laser validation and reference • Lower domestic steerage
reimbursement, if applicable
Friendship Village — Lockton Total Rewards Practice overview 22 Lockton Companies
management and stop-loss
Dedicated Clinical Claims Unit — Core value
Lockton’s clinical claims team is CLINICAL COST CONTAINMENT PATHWAY
made up of dedicated physicians,
nurses, billing and coding experts,
etc., as well as a strategic partnership
with the Mayo Clinic. Our clinical
review and management approach Stop-loss carrier
is complementary to processes
currently utilized by your carriers and
administrators. Below are examples of
our approach: YES, INFORM
• Focus on the small minority (<1%) CLAIMANT ACTIONABLE TPA/ASO RECOMMENDED TEAM/ IMPLEMENTATION
of cases that drive the greatest IDENTIFICATION STRATEGY
costs OPPORTUNITY CLIENT
• Depth of review and length of time
spent working cases that require
a highly resource-intensive model CCU
not feasible for many insurers
• Dedicated medical director with Complex Claims Clinical
deep expertise in provider quality Consulting Unit
management and cost containment
• Independent relationships with CLAIMS MANAGEMENT CLINICAL DASHBOARD COST CONTAINMENT
numerous providers and ability to
negotiate with both in- and out-of- • Ongoing claims tracking • Over 9,000 large claimants • Verify site of care
network providers • Monthly report monitoring identiied using available data • Review pharmacy utilization
• “Concurrent” specialty case review, • 85% identiication resources • Alternative treatment methods
if desired • Timely claim reimbursement • Track large claimants and group • Cost eficiency and alignment
• Access to specialty contracts trends
(e.g., transplant, ESRD, oncology, • Year-end claim reconciliation • Current and future claim • Domestic steerage, if applicable
pharmacy) • Team of physicians, nurses, billing projections • Custom managed care rates, if
and coding experts, etc. • Condition and treatment education applicable
• Laser validation and reference • Lower domestic steerage
reimbursement, if applicable
Friendship Village — Lockton Total Rewards Practice overview 22 Lockton Companies