Page 28 - 2021-2022 New Hire Benefits
P. 28
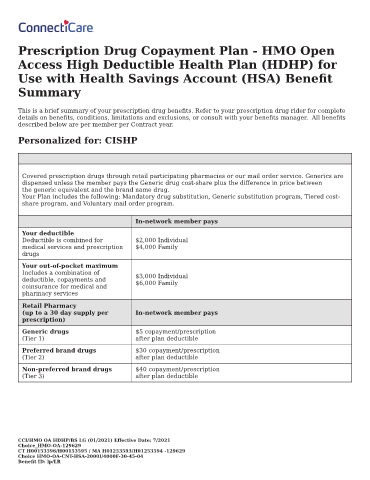
Prescription Drug Copayment Plan - HMO Open
Access High Deductible Health Plan (HDHP) for
Use with Health Savings Account (HSA) Bene t
Summary
This is a brief summary of your prescription drug bene ts. Refer to your prescription drug rider for complete
details on bene ts, conditions, limitations and exclusions, or consult with your bene ts manager. All bene ts
described below are per member per Contract year.
Personalized for: CISHP
Covered prescription drugs through retail participating pharmacies or our mail order service. Generics are
dispensed unless the member pays the Generic drug cost-share plus the di erence in price between
the generic equivalent and the brand name drug.
Your Plan includes the following: Mandatory drug substitution, Generic substitution program, Tiered cost-
share program, and Voluntary mail order program.
In-network member pays
Your deductible
Deductible is combined for $2,000 Individual
medical services and prescription $4,000 Family
drugs
Your out-of-pocket maximum
Includes a combination of $3,000 Individual
deductible, copayments and $6,000 Family
coinsurance for medical and
pharmacy services
Retail Pharmacy
(up to a 30 day supply per In-network member pays
prescription)
Generic drugs $5 copayment/prescription
(Tier 1) after plan deductible
Preferred brand drugs $30 copayment/prescription
(Tier 2) after plan deductible
Non-preferred brand drugs $40 copayment/prescription
(Tier 3) after plan deductible
CCI/HMO OA HDHP/BS LG (01/2021) E ective Date: 7/2021
Choice_HMO-OA-129629
CT H00153596/H00153595 / MA H01253593/H01253594 -129629
Choice HMO-OA-CNT-HSA-2000I/4000F-30-45-04
Bene t ID: lp/LR