Page 17 - Tampa Bay Rays 2022 Flipbook
P. 17
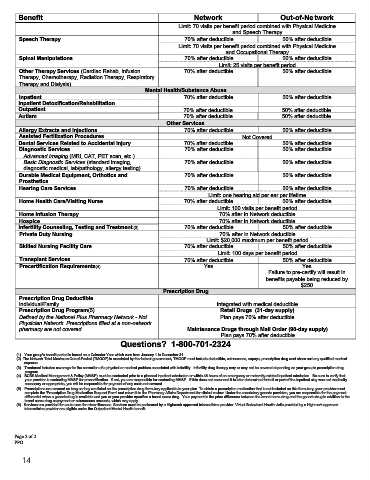
Benefit Network Out-of-Network
Limit: 70 visits per benefit period combined with Physical Medicine
and Speech Therapy
Speech Therapy 70% after deductible 50% after deductible
Limit: 70 visits per benefit period combined with Physical Medicine
and Occupational Therapy
Spinal Manipulations 70% after deductible 50% after deductible
Limit: 25 visits per benefit period
Other Therapy Services (Cardiac Rehab, Infusion 70% after deductible 50% after deductible
Therapy, Chemotherapy, Radiation Therapy, Respiratory
Therapy and Dialysis)
Mental Health/Substance Abuse
Inpatient 70% after deductible 50% after deductible
Inpatient Detoxification/Rehabilitation
Outpatient 70% after deductible 50% after deductible
Autism 70% after deductible 50% after deductible
Other Services
Allergy Extracts and injections 70% after deductible 50% after deductible
Assisted Fertilization Procedures Not Covered
Dental Services Related to Accidental Injury 70% after deductible 50% after deductible
Diagnostic Services 70% after deductible 50% after deductible
Advanced Imaging (MRI, CAT, PET scan, etc.)
Basic Diagnostic Services (standard imaging, 70% after deductible 50% after deductible
diagnostic medical, lab/pathology, allergy testing)
Durable Medical Equipment, Orthotics and 70% after deductible 50% after deductible
Prosthetics
Hearing Care Services 70% after deductible 50% after deductible
Limit: one hearing aid per ear per lifetime
Home Health Care/Visiting Nurse 70% after deductible 50% after deductible
Limit: 100 visits per benefit period
Home Infusion Therapy 70% after In Network deductible
Hospice 70% after In Network deductible
Infertility Counseling, Testing and Treatment(3) 70% after deductible 50% after deductible
Private Duty Nursing 70% after In Network deductible
Limit: $20,000 maximum per benefit period
Skilled Nursing Facility Care 70% after deductible 50% after deductible
Limit: 100 days per benefit period
Transplant Services 70% after deductible 50% after deductible
Precertification Requirements(4) Yes Yes
Failure to pre-certify will result in
benefits payable being reduced by
$250
Prescription Drug
Prescription Drug Deductible
Individual/Family Integrated with medical deductible
Prescription Drug Program(5) Retail Drugs (31-day supply)
Defined by the National Plus Pharmacy Network - Not Plan pays 70% after deductible
Physician Network. Prescriptions filled at a non-network
pharmacy are not covered. Maintenance Drugs through Mail Order (90-day supply)
Plan pays 70% after deductible
Questions? 1-800-701-2324
(1) Your group's benefit period is based on a Calendar Year which runs from January 1 to December 31.
(2) The Network Total Maximum Out-of-Pocket (TMOOP) is mandated by the federal government, TMOOP must include deductible, coinsurance, copays, prescription drug cost share and any qualified medical
expense.
(3) Treatment includes coverage for the correction of a physical or medical problem associated with infertility. Infertility drug therapy may or may not be covered depending on your group’s prescription drug
program.
(4) BCBS Medical Management & Policy (MM&P) must be contacted prior to a planned inpatient admission or within 48 hours of an emergency or maternity-related inpatient admission. Be sure to verify that
your provider is contacting MM&P for precertification. If not, you are responsible for contacting MM&P. If this does not occur and it is later determined that all or part of the inpatient stay was not medically
necessary or appropriate, you will be responsible for payment of any costs not covered.
(5) Prescriptions are covered as long as they are listed on the prescription drug formulary applicable to your plan. To obtain a prescription medication that is not included on this formulary, your provider must
complete the 'Prescription Drug Medication Request Form' and return it to the Pharmacy Affairs Department for clinical review. Under the mandatory generic provision, you are responsible for the payment
differential when a generic drug is available and you or your provider specifies a brand name drug. Your payment is the price difference between the brand name drug and the generic drug in addition to the
brand name drug copayment or coinsurance amounts, which may apply.
(6) Services are provided for acute care for minor illnesses. Services must be performed by a Highmark approved telemedicine provider. Virtual Behavioral Health visits provided by a Highmark approved
telemedicine provider are eligible under the Outpatient Mental Health benefit.
Page 2 of 2
PPO
14