Page 6 - GP Fall Final 2017
P. 6
Oral Lichen Planus
By Christine Macarelli, RDH, MS and Gwen Cohen Brown, DDS, FAAOMP
Introduction antifungal medications. An OLL can also Diagnosis
Lichen planus is a chronic mucocutaneous result from individuals who have a sensi- Diagnosis of OLP is established either by
disease of inflammatory origin that affects tivity to heavy metals. 2,3,4 direct visual and clinical examination or by
the dermis and lining mucosa. When pres- clinical examination with histopathologic
1
ent in the oral cavity, it is referred to as Clinical Appearance confirmation. To confirm the diagnosis of
1
oral lichen planus (OLP). It is estimated OLP most commonly presents in a bilateral, OLP versus the other conditions that pres-
that 50% of individuals who present with symmetrical pattern. The most frequent sites ent as a desquamative gingivitis, a biopsy
skin lichen planus will also have oral man- for clinical presentation of OLP include the is indicated.
ifestations of the disease. According to buccal mucosa, gingiva, tongue, and labial
2,3
the American Academy of Oral Medicine, mucosa. It is less commonly seen on the Etiologically, it is found that the basal cells
OLP affects approximately 2% of the pop- floor of the mouth, palate, and in the esopha- of epithelium are the targeted cells in lichen
ulation with the highest prevalence seen in geal area. While there are variations of OLP, planus and that the initial event is recogni-
1
women over the age of 50. It should be the three main types are reticular, atrophic tion of an antigen by mucosal Langerhans
1
noted that OLP has been seen in children, and erosive. Wickham striae, a reticular cells. Upon microscopic examination it is
2,4
but the occurrence is less likely. 1,4 variant, present as thin lacy lines and most found that there is a hyperkeratinization
often appear on the buccal mucosa. 5 of the superficial epithelium, the basal cell
Etiology and Pathogenesis layer appears to liquefy, and a thick band
OLP is a noninfectious condition in which Erosive or atrophic OLP can clinically be of lymphocytes are found subjacent to the
the cause is not clearly defined. Some re- confused with three other mucocutaneous epithelium in the lamina propria. 1
1
search suggests that the disease is an auto- conditions. Approximately 10% of patients
immune response; however, there are fac- with OLP have the disease confined to the Malignant Transformation
tors that appear to predispose an individual gingiva. Desquamative gingivitis is a con- Malignant transformation of OLP lesions
6
1
to OLP. These factors include a family dition where gingiva peel upon gentle or has been reported with a wide range of
history of the disease, psychological stress light pressure. This is also known as a pos- frequency. 9,10 An increased risk of oral
and systemic conditions such as Hepatitis itive Nikolsky sign. Other common condi- cancer developing in patients with OLP is
7
C, hypertension, diabetes, thyroid disease, tions which present desquamative gingivitis currently accepted, and is diagnosed on the
2
and stem cell transplant recipients. To are: Pemphigus Vulgaris, Benign Mucous basis of clinical and histological manifesta-
10
complicate matters, oral lichenoid lesions Membrane Pemphigoid and Erythema Mul- tions . The range of occurrence varies be-
(OLL) can have the clinical presentation tiforme. Less often, Dermatitis Herpeti- tween studies, but the range can go as high
6
of OLP. OLL can result from common formis, a condition associated with Crohn’s as 3.7%. Due to the potential transforma-
10
2
systemic drugs such as NSAID’s, antihy- disease, and Linear IgA Bullous Dermatosis tion of OLP to squamous cell carcinoma,
pertensive, hypoglycemic, antibiotics, and also exhibit desquamative gingivitis. patients with OLP should be monitored
8
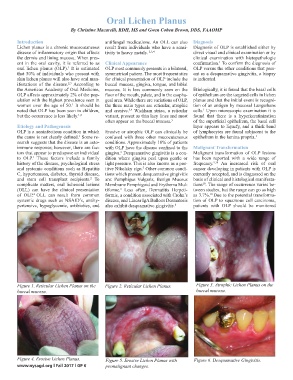
Figure 1. Reticular Lichen Planus on the Figure 2. Reticular Lichen Planus. Figure 3. Atrophic Lichen Planus on the
buccal mucosa. buccal mucosa.
Figure 4. Erosive Lichen Planus. Figure 5. Erosive Lichen Planus with Figure 6. Desquamative Gingivitis.
www.nysagd.org l Fall 2017 l GP 6 premalignant changes.