Page 1345 - draft
P. 1345
2021
Your Medical Options Dental Plans
Blue Cross and Blue Shield of Illinois Aetna Dental
Blue Cross and Blue Shield of Illinois (BCBSIL) is the claims Log in to your secure member website at www.aetna.com to
administrator for your district’s medical plan(s). explore the resources available to you. Call 877.238.6200 if
Contact Blue Cross for questions regarding: you have any questions— 24 hours a day, 365 days a year.
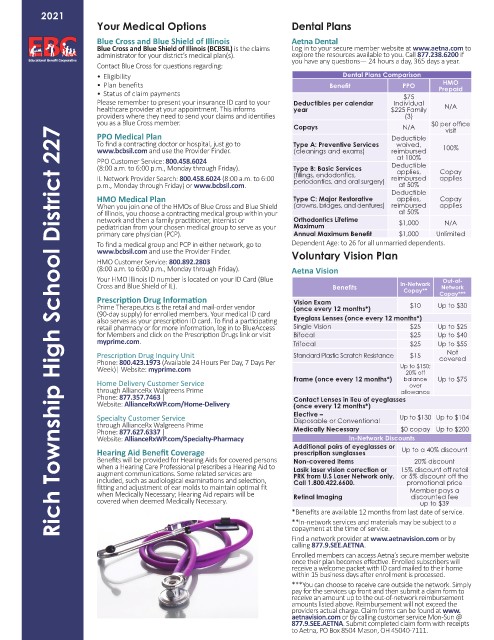
• Eligibility Dental Plans Comparison
HMO
• Plan benefits Benefit PPO Prepaid
• Status of claim payments $75
Please remember to present your insurance ID card to your Deductibles per calendar Individual
healthcare provider at your appointment. This informs year $225 Family N/A
providers where they need to send your claims and identifies (3)
you as a Blue Cross member. $0 per office
Copays N/A visit
Rich Township High School District 227
PPO Medical Plan Deductible
To find a contracting doctor or hospital, just go to Type A: Preventive Services waived,
www.bcbsil.com and use the Provider Finder. (cleanings and exams) reimbursed 100%
PPO Customer Service: 800.458.6024 at 100%
(8:00 a.m. to 6:00 p.m., Monday through Friday). Type B: Basic Services Deductible Copay
applies,
IL Network Provider Search: 800.458.6024 (8:00 a.m. to 6:00 (fillings, endodontics, reimbursed applies
periodontics, and oral surgery)
p.m., Monday through Friday) or www.bcbsil.com. at 50%
Deductible
HMO Medical Plan Type C: Major Restorative applies, Copay
When you join one of the HMOs of Blue Cross and Blue Shield (crowns, bridges, and dentures) reimbursed applies
of Illinois, you choose a contracting medical group within your at 50%
network and then a family practitioner, internist or Orthodontics Lifetime $1,000 N/A
pediatrician from your chosen medical group to serve as your Maximum
primary care physician (PCP). Annual Maximum Benefit $1,000 Unlimited
To find a medical group and PCP in either network, go to Dependent Age: to 26 for all unmarried dependents.
www.bcbsil.com and use the Provider Finder. Voluntary Vision Plan
HMO Customer Service: 800.892.2803
(8:00 a.m. to 6:00 p.m., Monday through Friday). Aetna Vision
Your HMO Illinois ID number is located on your ID Card (Blue Out-of-
Cross and Blue Shield of IL). Benefits In-Network Network
Copay**
Prescription Drug Information Vision Exam Copay***
Prime Therapeutics is the retail and mail-order vendor (once every 12 months*) $10 Up to $30
(90-day supply) for enrolled members. Your medical ID card
also serves as your prescription ID card. To find a participating Eyeglass Lenses (once every 12 months*)
retail pharmacy or for more information, log in to BlueAccess Single Vision $25 Up to $25
for Members and click on the Prescription Drugs link or visit Bifocal $25 Up to $40
myprime.com. Trifocal $25 Up to $55
Not
Prescription Drug Inquiry Unit Standard Plastic Scratch Resistance $15 covered
Phone: 800.423.1973 (Available 24 Hours Per Day, 7 Days Per
Week)| Website: myprime.com Up to $150;
20% off
Home Delivery Customer Service Frame (once every 12 months*) balance Up to $75
over
through AllianceRx Walgreens Prime allowance
Phone: 877.357.7463 | Contact Lenses in lieu of eyeglasses
Website: AllianceRxWP.com/Home-Delivery (once every 12 months*)
Specialty Customer Service Elective – Up to $130 Up to $104
Disposable or Conventional
through AllianceRx Walgreens Prime
Phone: 877.627.6337 | Medically Necessary $0 copay Up to $200
Website: AllianceRxWP.com/Specialty-Pharmacy In-Network Discounts
Additional pairs of eyeglasses or
Hearing Aid Benefit Coverage prescription sunglasses Up to a 40% discount
Benefits will be provided for Hearing Aids for covered persons Non-covered items 20% discount
when a Hearing Care Professional prescribes a Hearing Aid to Lasik laser vision correction or 15% discount off retail
augment communications. Some related services are PRK from U.S Laser Network only. or 5% discount off the
included, such as audiological examinations and selection, Call 1.800.422.6600. promotional price
fitting and adjustment of ear molds to maintain optimal fit Member pays a
when Medically Necessary; Hearing Aid repairs will be Retinal Imaging discounted fee
covered when deemed Medically Necessary. up to $39
*Benefits are available 12 months from last date of service.
**In-network services and materials may be subject to a
copayment at the time of service.
Find a network provider at www.aetnavision.com or by
calling 877.9.SEE.AETNA.
Enrolled members can access Aetna’s secure member website
once their plan becomes effective. Enrolled subscribers will
receive a welcome packet with ID card mailed to their home
within 15 business days after enrollment is processed.
***You can choose to receive care outside the network. Simply
pay for the services up front and then submit a claim form to
receive an amount up to the out-of-network reimbursement
amounts listed above. Reimbursement will not exceed the
providers actual charge. Claim forms can be found at www.
aetnavision.com or by calling customer service Mon-Sun @
877.9.SEE.AETNA. Submit completed claim form with receipts
to Aetna, PO Box 8504 Mason, OH 45040-7111.