Page 483 - Fluid, Electrolyte, and Acid-Base Disorders in Small Animal Practice
P. 483
Fluid, Electrolyte, and Acid-Base Disturbances in Liver Disease 471
Portal hypertension Portosystemic shunting
iNOS Nitric oxide Acquired PSS
Vasodilated large varices Hypoalbuminemia
Transmural bacterial
passage splanchnic circulation 3rd space
Peripheral arterial Arteriovenous shunts Synthesis
Endotoxins vasodilatation (splanchnic and pulmonary) distribution Loss into
intestine:
Vasodilatory effects: Peripheral PLE
peptides: glucagon, VIP, Catabolism vasodilatation:
bile salts, prostaglandins, Gravitational pooling Dilution
local autonomic tone “Vascular underfilling” (splanchnic vasculature)
Signals sodium and Non-osmotic baroreceptors
water conservation Free cortisol
Sympathetic nervous system Vasopressin Bile salts ACTH
Renal
angiotensin II Renin-angiotensin-aldosterone Inhibition
11 -hydroxysteroid
dehydrogenase
Cardiac output
Efferent Vasoconstriction Vasodilatory “Apparent”
arteriole renal prostaglandins Hyperdynamic Abnormal release mineralocorticoid
mineralocorticoid
circulatory excess
Filtration fraction syndrome
Perfusion redistribution:
Filtrate absorption: Cortex Juxtaglomerular Aldosterone
proximal tubule tubules escape
Renal sodium
GFR Impaired excretion
Peritubular solute-free H 2 O retention
fluid and sodium resorption
Adequately normalizes Fails to normalize
Renal sodium and H 2 O circulatory homeostasis Plasma volume circulatory homeostasis
retention
Portal hypertension/lymph formation
Normalization Persistent activation
Intrahepatic portal Na and H 2 O Na and H 2 O
hypertension retaining systems retaining systems
Fluid exudation from
Up to 10 increase in splanchnic/visceral Normal excretion: Continued retention: Renal
hepatic lymph formation Na and H 2 O Na and H 2 O vasoconstriction
lymphatics
Fluid “weeping” from Functional
hepatic capsule No ascites Ascites renal insufficiency
HEPATORENAL SYNDROME
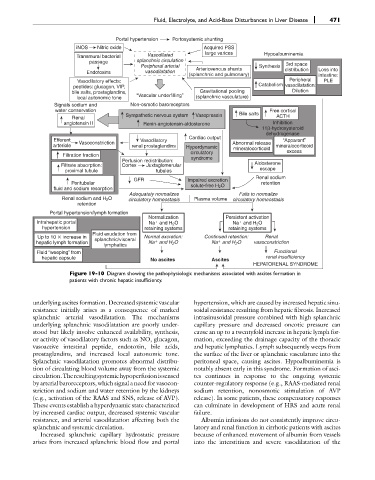
Figure 19-10 Diagram showing the pathophysiologic mechanisms associated with ascites formation in
patients with chronic hepatic insufficiency.
underlying ascites formation. Decreased systemic vascular hypertension, which are caused by increased hepatic sinu-
resistance initially arises as a consequence of marked soidal resistance resulting from hepatic fibrosis. Increased
splanchnic arterial vasodilatation. The mechanisms intrasinusoidal pressure combined with high splanchnic
underlying splanchnic vasodilatation are poorly under- capillary pressure and decreased oncotic pressure can
stood but likely involve enhanced availability, synthesis, cause an up to a twentyfold increase in hepatic lymph for-
or activity of vasodilatory factors such as NO, glucagon, mation, exceeding the drainage capacity of the thoracic
vasoactive intestinal peptide, endotoxin, bile acids, and hepatic lymphatics. Lymph subsequently weeps from
prostaglandins, and increased local autonomic tone. the surface of the liver or splanchnic vasculature into the
Splanchnic vasodilatation promotes abnormal distribu- peritoneal space, causing ascites. Hypoalbuminemia is
tion of circulating blood volume away from the systemic notably absent early in this syndrome. Formation of asci-
circulation.Theresultingsystemichypoperfusionissensed tes continues in response to the ongoing systemic
by arterial baroreceptors, which signal a need for vasocon- counter-regulatory response (e.g., RAAS-mediated renal
striction and sodium and water retention by the kidneys sodium retention, nonosmotic stimulation of AVP
(e.g., activation of the RAAS and SNS, release of AVP). release). In some patients, these compensatory responses
These events establish a hyperdynamic state characterized can culminate in development of HRS and acute renal
by increased cardiac output, decreased systemic vascular failure.
resistance, and arterial vasodilatation affecting both the Albumin infusions do not consistently improve circu-
splanchnic and systemic circulation. latory and renal function in cirrhotic patients with ascites
Increased splanchnic capillary hydrostatic pressure because of enhanced movement of albumin from vessels
arises from increased splanchnic blood flow and portal into the interstitium and severe vasodilatation of the