Page 3 - 06- Cirrhosis of the Liver
P. 3
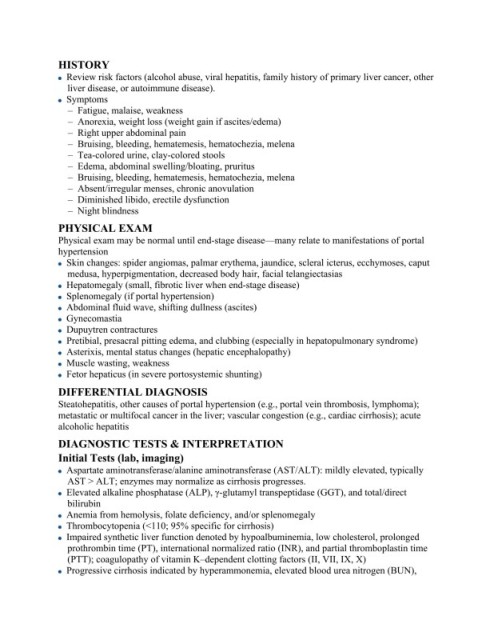
HISTORY
Review risk factors (alcohol abuse, viral hepatitis, family history of primary liver cancer, other
liver disease, or autoimmune disease).
Symptoms
– Fatigue, malaise, weakness
– Anorexia, weight loss (weight gain if ascites/edema)
– Right upper abdominal pain
– Bruising, bleeding, hematemesis, hematochezia, melena
– Tea-colored urine, clay-colored stools
– Edema, abdominal swelling/bloating, pruritus
– Bruising, bleeding, hematemesis, hematochezia, melena
– Absent/irregular menses, chronic anovulation
– Diminished libido, erectile dysfunction
– Night blindness
PHYSICAL EXAM
Physical exam may be normal until end-stage disease—many relate to manifestations of portal
hypertension
Skin changes: spider angiomas, palmar erythema, jaundice, scleral icterus, ecchymoses, caput
medusa, hyperpigmentation, decreased body hair, facial telangiectasias
Hepatomegaly (small, fibrotic liver when end-stage disease)
Splenomegaly (if portal hypertension)
Abdominal fluid wave, shifting dullness (ascites)
Gynecomastia
Dupuytren contractures
Pretibial, presacral pitting edema, and clubbing (especially in hepatopulmonary syndrome)
Asterixis, mental status changes (hepatic encephalopathy)
Muscle wasting, weakness
Fetor hepaticus (in severe portosystemic shunting)
DIFFERENTIAL DIAGNOSIS
Steatohepatitis, other causes of portal hypertension (e.g., portal vein thrombosis, lymphoma);
metastatic or multifocal cancer in the liver; vascular congestion (e.g., cardiac cirrhosis); acute
alcoholic hepatitis
DIAGNOSTIC TESTS & INTERPRETATION
Initial Tests (lab, imaging)
Aspartate aminotransferase/alanine aminotransferase (AST/ALT): mildly elevated, typically
AST > ALT; enzymes may normalize as cirrhosis progresses.
Elevated alkaline phosphatase (ALP), γ-glutamyl transpeptidase (GGT), and total/direct
bilirubin
Anemia from hemolysis, folate deficiency, and/or splenomegaly
Thrombocytopenia (<110; 95% specific for cirrhosis)
Impaired synthetic liver function denoted by hypoalbuminemia, low cholesterol, prolonged
prothrombin time (PT), international normalized ratio (INR), and partial thromboplastin time
(PTT); coagulopathy of vitamin K–dependent clotting factors (II, VII, IX, X)
Progressive cirrhosis indicated by hyperammonemia, elevated blood urea nitrogen (BUN),