Page 5 - 06- Cirrhosis of the Liver
P. 5
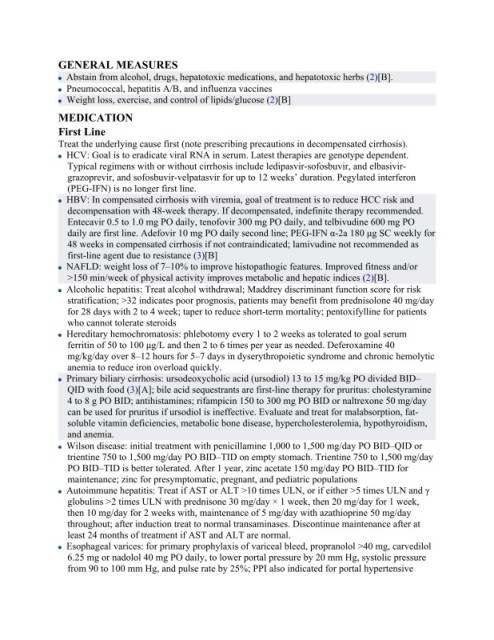
GENERAL MEASURES
Abstain from alcohol, drugs, hepatotoxic medications, and hepatotoxic herbs (2)[B].
Pneumococcal, hepatitis A/B, and influenza vaccines
Weight loss, exercise, and control of lipids/glucose (2)[B]
MEDICATION
First Line
Treat the underlying cause first (note prescribing precautions in decompensated cirrhosis).
HCV: Goal is to eradicate viral RNA in serum. Latest therapies are genotype dependent.
Typical regimens with or without cirrhosis include ledipasvir-sofosbuvir, and elbasivir-
grazoprevir, and sofosbuvir-velpatasvir for up to 12 weeks’ duration. Pegylated interferon
(PEG-IFN) is no longer first line.
HBV: In compensated cirrhosis with viremia, goal of treatment is to reduce HCC risk and
decompensation with 48-week therapy. If decompensated, indefinite therapy recommended.
Entecavir 0.5 to 1.0 mg PO daily, tenofovir 300 mg PO daily, and telbivudine 600 mg PO
daily are first line. Adefovir 10 mg PO daily second line; PEG-IFN α-2a 180 μg SC weekly for
48 weeks in compensated cirrhosis if not contraindicated; lamivudine not recommended as
first-line agent due to resistance (3)[B]
NAFLD: weight loss of 7–10% to improve histopathogic features. Improved fitness and/or
>150 min/week of physical activity improves metabolic and hepatic indices (2)[B].
Alcoholic hepatitis: Treat alcohol withdrawal; Maddrey discriminant function score for risk
stratification; >32 indicates poor prognosis, patients may benefit from prednisolone 40 mg/day
for 28 days with 2 to 4 week; taper to reduce short-term mortality; pentoxifylline for patients
who cannot tolerate steroids
Hereditary hemochromatosis: phlebotomy every 1 to 2 weeks as tolerated to goal serum
ferritin of 50 to 100 μg/L and then 2 to 6 times per year as needed. Deferoxamine 40
mg/kg/day over 8–12 hours for 5–7 days in dyserythropoietic syndrome and chronic hemolytic
anemia to reduce iron overload quickly.
Primary biliary cirrhosis: ursodeoxycholic acid (ursodiol) 13 to 15 mg/kg PO divided BID–
QID with food (3)[A]; bile acid sequestrants are first-line therapy for pruritus: cholestyramine
4 to 8 g PO BID; antihistamines; rifampicin 150 to 300 mg PO BID or naltrexone 50 mg/day
can be used for pruritus if ursodiol is ineffective. Evaluate and treat for malabsorption, fat-
soluble vitamin deficiencies, metabolic bone disease, hypercholesterolemia, hypothyroidism,
and anemia.
Wilson disease: initial treatment with penicillamine 1,000 to 1,500 mg/day PO BID–QID or
trientine 750 to 1,500 mg/day PO BID–TID on empty stomach. Trientine 750 to 1,500 mg/day
PO BID–TID is better tolerated. After 1 year, zinc acetate 150 mg/day PO BID–TID for
maintenance; zinc for presymptomatic, pregnant, and pediatric populations
Autoimmune hepatitis: Treat if AST or ALT >10 times ULN, or if either >5 times ULN and γ
globulins >2 times ULN with prednisone 30 mg/day × 1 week, then 20 mg/day for 1 week,
then 10 mg/day for 2 weeks with, maintenance of 5 mg/day with azathioprine 50 mg/day
throughout; after induction treat to normal transaminases. Discontinue maintenance after at
least 24 months of treatment if AST and ALT are normal.
Esophageal varices: for primary prophylaxis of variceal bleed, propranolol >40 mg, carvedilol
6.25 mg or nadolol 40 mg PO daily, to lower portal pressure by 20 mm Hg, systolic pressure
from 90 to 100 mm Hg, and pulse rate by 25%; PPI also indicated for portal hypertensive