Page 18 - e-book CPG - Bipolar Disorder (full 92 pg) (1)
P. 18
CLINICAL PRACTICE GUIDELINES MANAGEMENT OF BIPOLAR DISORDER (2ND ED.)
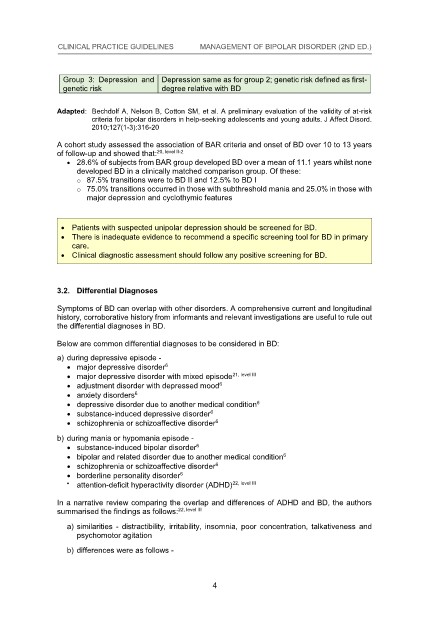
Group 3: Depression and Depression same as for group 2; genetic risk defined as first-
genetic risk Depression and Depression same as for group 2; genetic risk defined as first-
Group 3: degree relative with BD
genetic risk degree relative with BD
Group 3: Depression and Depression same as for group 2; genetic risk defined as first-
Adapted: Bechdolf A, Nelson B, Cotton SM, et al. A preliminary evaluation of the validity of at-risk
degree relative with BD
genetic risk
Group 3: Depression and Depression same as for group 2; genetic risk defined as first-
criteria for bipolar disorders in help-seeking adolescents and young adults. J Affect Disord.
Adapted: Bechdolf A, Nelson B, Cotton SM, et al. A preliminary evaluation of the validity of at-risk
Group 3: Depression and Depression same as for group 2; genetic risk defined as first-
2010;127(1-3):316-20 degree relative with BD
genetic risk
Adapted: Bechdolf A, Nelson B, Cotton SM, et al. A preliminary evaluation of the validity of at-risk
criteria for bipolar disorders in help-seeking adolescents and young adults. J Affect Disord.
Group 3: Depression and Depression same as for group 2; genetic risk defined as first-
genetic risk degree relative with BD
Group 3: Depression and Depression same as for group 2; genetic risk defined as first-
criteria for bipolar disorders in help-seeking adolescents and young adults. J Affect Disord.
sk
genetic ri 2010;127(1-3):316-20 degree relative with BD
Group 3: Depression and
2010;127(1-3):316-20 Depression same as for group 2; genetic risk defined as first-
Adapted: Bechdolf A, Nelson B, Cotton SM, et al. A preliminary evaluation of the validity of at-risk
A cohort study assessed the association of BAR criteria and onset of BD over 10 to 13 years
degree relative with BD
genetic risk
Adapted: Bechdolf A, Nelson B, Cotton SM, et al. A preliminary evaluation of the validity of at-risk
criteria for bipolar disorders in help-seeking adolescents and young adults. J Affect Disord.
degree
genetic risk 20, level II-2relative with BD
SM, et al. A preliminary evaluation of the validity of at-risk
of follow-up and showed that:
Adapted: Bechdolf A, Nelson B, Cotton
A cohort study assessed the association of BAR criteria and onset of BD over 10 to 13 years
criteria for bipolar disorders in help-seeking adolescents and young adults. J Affect Disord.
2010;127(1-3):316-20
Adapted: Bechdolf A, Nelson B, Cotton SM, et al. A preliminary evaluation of the validity of at-risk
criteria for bipolar disorders in help-seeking adolescents and young adults. J Affect Disord.
A cohort study assessed the association of BAR criteria and onset of BD over 10 to 13 years
28.6% of subjects from BAR group developed BD over a mean of 11.1 years whilst none
of follow-up and showed that:
2010;127(1-3):316-20 20, level II-2
Adapted: Bechdolf A, Nelson B, Cotton SM, et al. A preliminary evaluation of the validity of at-risk
criteria for bipolar disorders in help-seeking adolescents and young adults. J Affect Disord.
2010;127(1-3):316-20
of follow-up and showed that:
20, level II-2
developed BD in a clinically matched comparison group. Of these: .1 years whilst none
28.6% of subjects from BAR group developed BD over a mean of 11
criteria for bipolar disorders in help-seeking adolescents and young adults. J Affect Disord.
A cohort study assessed the association of BAR criteria and onset of BD over 10 to 13 years
2010;127(1-3):316-20
28.6% of subjects from BAR group developed BD over a mean of 11.1 years whilst none
A cohort study assessed the association of BAR criteria and onset of BD over 10 to 13 years
o 87.5% transitions were to BD II and 12.5% to BD I p. Of these:
developed BD in a clinically matched comparison grou
of follow-up and showed that:
2010;127(1-3):316-20 20, level II-2
A cohort study assessed the association of BAR criteria and onset of BD over 10 to 13 years
developed BD in a clinically matched comparison group. Of these:
of follow-up and showed that:
o 87.5% transitions were to BD II and 12.5% to BD I
20, level II-2
o 75.0% transitions occurred in those with subthreshold mania and 25.0% in those with
28.6% of subjects from BAR group developed BD over a mean of 11.1 years whilst none
A cohort study assessed the association of BAR criteria and onset of BD over 10 to 13 years
of follow-up and showed that:
20, level II-2
o 87.5% transitions were to BD II and 12.5% to BD I
major depression and cyclothymic features D over a mean of 11.1 years whilst none
28.6% of subjects from BAR group developed B
A cohort study assessed the association of BAR criteria and onset of BD over 10 to 13 years
o 75.0% transitions occurred in those with subthreshold mania and 25.0% in those with
of follow-up and showed that:
developed BD in a clinically matched comparison group. Of these:
20, level II-2
28.6% of subjects from BAR group developed BD over a mean of 11.1 years whilst none
o 75.0% transitions occurred in those with subthreshold mania and 25.0% in those with
major depression an
of follow-up and showed that:d cyclothymic features
developed BD in a clinically matched comparison group. Of these:
20, level II-2
28.6% of subjects from BAR group developed BD over a mean of 11.1 years whilst none
o 87.5% transitions were to BD II and 12.5% to BD I
developed BD in a clinically matched comparison group. Of these:
major depression and cyclothymic features
o 87.5% transitions were to BD II and 12.5% to BD I
28.6% of subjects from BAR group developed BD over a mean of 11.1 years whilst none
developed BD in a clinically matched comparison group. Of these:
o 75.0% transitions occurred in those with subthreshold mania and 25.0% in those with
o 87.5% transitions were to BD II and 12.5% to BD I
Patients with suspected unipolar depression should be screened for BD.
o 75.0% transitions occurred in those with subthreshold mania and 25.0% in those with
developed BD in a clinically matched comparison group. Of these:
major depression and cyclothymic features
o 87.5% transitions were to BD II and 12.5% to BD I
There is inadequate evidence to recommend a specific screening tool for BD in primary
o 75.0% transitions occurred in those with subthreshold mania and 25.0% in those with
Patients with suspected unipolar depression should be screened for BD.
major depression and cyclothymic features
o 87.5% transitions were to BD II and 12.5% to BD I
o 75.0% transitions occurred in those with subthreshold mania and 25.0% in those with
Patients with suspected unipolar depression should be screened for BD.
care. major depression and cyclothymic features
There is inadequate evidence to recommend a specific screening tool for BD in primary
o 75.0% transitions occurred in those with subthreshold mania and 25.0% in those with
major depression and cyclothymic features
There is inadequate evidence to recommend a specific screening tool for BD in primary
care.
Clinical diagnostic assessment should follow any positive screening for BD.
Patients with suspected unipolar depression should be screened for BD.
major depression and cyclothymic features
care.
Patients with suspected unipolar depression should be screened for BD.
Clinical diagnostic assessment should follow any positive screening for BD.
There is inadequate evidence to recommend a specific screening tool for BD in primary
Patients with suspected unipolar depression should be screened for BD.
Clinical diagnostic assessment should follow any positive screening for BD.
There is inadequate evidence to recommend a specific screening tool for BD in primary
care.
Patients with suspected unipolar depression should be screened for BD.
3.2. Differential Diagnoses
There is inadequate evidence to recommend a specific screening tool for BD in primary
care.
Patients with suspected unipolar depression should be screened for BD.
There is inadequate evidence to recommend a specific screening tool for BD in primary
Clinical diagnostic assessment should follow any positive screening for BD.
care.
3.2. Differential Diagnoses
Clinical diagnostic assessment should follow any positive screening for BD.
There is inadequate evidence to recommend a specific screening tool for BD in primary
care.
3.2. Differential Diagnoses
Symptoms of BD can overlap with other disorders. A comprehensive current and longitudinal
Clinical diagnostic assessment should follow any positive screening for BD.
care.
Clinical diagnostic assessment should follow any positive screening for BD.
Symptoms of BD can overlap with other disorders. A comprehensive current and longitudinal
history, corroborative history from informants and relevant investigations are useful to rule out
3.2. Differential Diagnoses
Clinical diagnostic assessment should follow any positive screening for BD.
Symptoms of BD can overlap with other disorders. A comprehensive current and longitudinal
3.2. Differential Diagnoses
the differential diagnoses in BD.
history, corroborative history from informants and relevant investigations are useful to rule out
3.2. Differential Diagnoses
history, corroborative history from informants and relevant investigations are useful to rule out
the differential diagnoses in BD.
Symptoms of BD can overlap with other disorders. A comprehensive current and longitudinal
3.2. Differential Diagnoses
the differential diagnoses in BD.
Symptoms of BD can overlap with other disorders. A comprehensive current and longitudinal
3.2. Differential Diagnoses
Below are common differential diagnoses to be considered in BD:
history, corroborative history from informants and relevant investigations are useful to rule out
Symptoms of BD can overlap with other disorders. A comprehensive current and longitudinal
a) during depressive episode -
history, corroborative history from informants and relevant investigations are useful to rule out
Below are common differential diagnoses to be considered in BD:
Symptoms of BD can overlap wit
the differential diagnoses in BD. h other disorders. A comprehensive current and longitudinal
history, corroborative history from informants and relevant investigations are useful to rule out
Below are common differential diagnoses to be considered in BD:
the differential diagnoses in BD.
6
Symptoms of BD can overlap with other disorders. A comprehensive current and longitudinal
a) during depressive episode -
major depressive disorder
history, corroborative history from informants and relevant investigations are useful to rule out
the differential diagnoses in BD.
major depressive disorder
major depressive disorder with mixed episode
history, corroborative history from informants and relevant investigations are useful to rule out
a) during depressive episode - 6
21, level III
the differential diagnoses in BD.
Below are common differential diagnoses to be considered in BD:
major depressive disorder
the differential diagnoses in BD.
Below are common differential diagnoses to be considered in BD:
major depressive disorder with mixed episode
adjustment disorder with depressed mood
6
a) during depressive episode -
Below are common differential diagnoses to be considered
21, level III in BD:
major depressive disorder with mixed episode
a) during depressive epi
adjustment disorde
anxiety disorders r with depressed mood
6
Below are common differential diagnoses to be considered in BD:
major depressive disorder
a) during depressive episode -
major depressive disorder
adjustment disorder with depressed mood
6
Below are common differential diagnoses to be considered in BD:
anxiety disorders
depressive disorder due to another medical condition
6
a) during depressive episode -
major depressive disorder with mixed episode
21, level III
major depressive disorder
major depressive disorder with mixed epi
a) during depressive epi 6sode - 6 6 6 6 6with mixed episode 21, level III 6 6 6
6sode
21, level III
6
anxiety disorders sode - 6
21, level III
depressive disorder due to another medical condition
major depressive disorder
adjustment disorder with depressed mood
substance-induced depressive disorder 6
major depressive disorder
major depressive disorder pressed mood
6
adjustment disorder with de
depressive disorder due to another medical condition
6
substance-induced depressive disorder
6
major depressive disorder with mixed episode
anxiety disorders
6
adjustment disorder with depressed mood
schizophrenia or schizoaffective disorder 6
substance-induced depressive disorder sode
6
21, level III
anxiety disorders
schizophrenia or schizoaffective disorder
adjustment disorder with depressed mood
b) during mania or hypomania episode - 6 6 21, level III 6
major depressive disorder with mixed epi 6
depressive disorder due to another medical condition
anxiety disorders
6
adjustment disorder with depressed mood
schizophrenia or schizoaffective disorder condition
depressive disorder due to another medical
substance-induced bipolar disorder
b) during mania or hypomania episode - 6 6 6 6 6 6
6
anxiety disorders
substance-induced depressive disorder
depressive disorder due to another med
anxiety disorders
substance-induced depressive disorder
6
6
b) during mania or hypomania episode - 6 6ical condition 6
substance-induced bipolar disorder
bipolar and related disorder due to another medical condition
depressive disorder due to another med
6ical condition
6
substance-induced depressive disorder
schizophrenia or schizoaffective disorder
depressive disorder due to another medical condition
substance-induced bipolar disorder
6
schizophrenia or schizoaffective disorder
schizophrenia or schizoaffective disorder
bipolar and related disorder due to another medical condition
substance-induced depressive disorder
6
b) during mania or hypomania episode - 6 6 6 6 6 6
schizophrenia or schizoaffective disorder
bipolar and related disorder duee -
b) during mania or hypomania episod 6 to another medical condition
6
schizophrenia or schizoaffective disorder
substance-induced depressive disorder 6 6
schizophrenia or schizoaffective disorder
borderline personality disorder
6
substance-induced bipolar disorder
b) during mania or hypomania episode - 6 6 6 22, level III
schizophrenia or schizoaffective disorder
substance-induced bipolar disorder
schizophrenia or schizoaffective disorder
6
borderline personality disorder
attention-deficit hyperactivity disorder (ADHD)
b) during mania or hypomania episode - 6 6
bipolar and related disorder due to another medical condition
substance-induced bipolar disorder
b) during mania or hypomania episod to another medical condition
6
bipolar and related disorder due
6
22, level III
attention-deficit hyperactivity disorder (ADHD)
substance-induced bipolar disorder
borderline personality disorder e - 6
schizophrenia or schizoaffective disorder
6
6
bipolar and related disorder due to another medical condition
22, level III
6
6
attention-deficit hyperactivity disorder (ADHD)
schizophrenia or schizoaffective disorder
substance-induced bipolar disorder
In a narrative review comparing the overlap and differences of ADHD and BD, the authors
bipolar and related disorder due to another medical condition
6
borderline personality disorder
6
schizophrenia or schizoaffective disorder
6
bipolar and related disorder due to another medical condition
borderline personality disorder
In a narrative review comparing the 6 22, level III 6 22, level III 6
summarised the findings as follows: overlap and differences of ADHD and BD, the authors
schizophrenia or schizoaffective disorder
attention-deficit hyperactivity disorder (ADHD)
6
borderline personality disorder
In a narrative review comparing the overlap and differences of ADHD and BD, the authors
22, level III
6
attention-deficit hyperactivity disorder (ADHD)
schizophrenia or schizoaffective disorder
22, level III
summarised the findings as follows:
a) similarities - distractibility, irritability, insomnia, poor concentration, talkativeness and
borderline personality disorder
6
attention-deficit hyperactivity disorder (ADHD)
borderline personality disorder
summarised the findings as follows: 6 22, level III 22, level III
a) similarities - distractibil
psychomotor agitation ity, irritability, insomnia, poor concentration, talkativeness and
In a narrative review comparing the overlap and differences of ADHD and BD, the authors
22, level III
attention-deficit hyperactivity disorder (ADHD)
narrative review comparing the overlap and differences of ADHD and BD, the authors
a) similarities - distractibility, irritability, insomnia, poor concentration, talkativeness and
attention-deficit hyperactivity disorder (ADHD)
In a psychomotor agitation
22, level III
summarised the findings as follows:
b) differences were as follows - 22, level III
In a narrative review comparing the overlap and differences of ADHD and BD, the authors
psychomotor agitation
22, level III
summarised the findings as follows:
b) differences were as follows -
In a narrative review comparing the overlap and differences of ADHD and BD, the authors
a) similarities - distractibility, irritability, insomnia, poor concentration, talkativeness and
summarised the findings as follows:
22, level III
In a narrative review comparing irritability, insomnia, poor concentration, talkativeness and
a) similarities - distractibility,
b) differences were as follows - the overlap and differences of ADHD and BD, the authors
22, level III
psychomotor agitation
a) similarities - distractibility, irritability,
psychomotor agitation
summarised the findings as follows:
summarised the findings as follows: 22, level III insomnia, poor concentration, talkativeness and
b) differences were as follows - irritability, insomnia, poor concentration, talkativeness and
a) similarities - distractibility,
psychomotor agitation
a) similarities - distractibility, irritability, insomnia, poor concentration, talkativeness and
b) differences were as follows -
psychomotor agitation
b) differences were as follows -
psychomotor agitation
b) differences were as follows -
b) differences were as follows -
4 4
4
4
4
4
4
4
4