Page 19 - e-book CPG - Bipolar Disorder (full 92 pg) (1)
P. 19
CLINICAL PRACTICE GUIDELINES MANAGEMENT OF BIPOLAR DISORDER (2ND ED.)
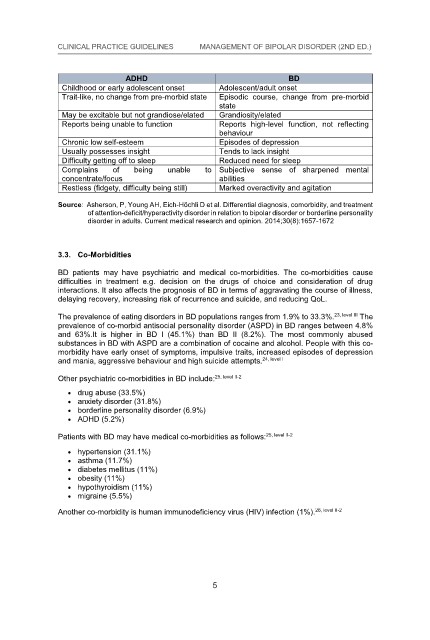
ADHD BD
BD
ADHD
Childhood or early adolescent onset Adolescent/adult onset
Childhood or early adolescent onset Adolescent/adult onset
Episodic course, change from pre-morbid
Trait-like, no change from pre-morbid state
BD
ADHD
Trait-like, no change from pre-morbid state Episodic course, change from pre-morbid
ADHD
BD
Adolescent/adult onset
Childhood or early adolescent onset state BD
state
ADHD
Childhood or early adolescent onset Adolescent/adult onset
May be excitable but not grandiose/elated
Grandiosity/elated
ADHD
Grandiosity/elated BD
Episodic course, change from pre-morbid
Trait-like, no change from pre-morbid state
May be excitable but not grandiose/elated
Childhood or early adolescent onset
Adolescent/adult onset
Episodic course, change from pre-morbid
Trait-like, no change from pre-morbid state
Reports high-level function, not reflecting
Reports being unable to function
Reports being unable to function set
Childhood or early adolescent on
Adolescent/adult onset
Reports high-level function, not reflecting
Episodic course, change from pre-morbid
Trait-like, no change from pre-morbid state
state
behaviour
Grandiosity/elated
Episodic
behaviour course, change from pre-morbid
Trait-like, no change from pre-morbid state
May be excitable but not grandiose/elated state
state
Episodes of depression
Grandiosity/elated
May be excitable but not grandiose/elated
Chronic low self-esteem unable to Subjective sense of
Reports being unable to
Chronic low self-esteem function
state
Episodes of depression
Reports high-level function, not reflecting
May be excitable but not grandiose/elated
Grandiosity/elated
Tends to lack insight
Reports high-level function, not reflecting
Reports being unable to function
Usually possesses insight
behaviour
Grandiosity/elated
May be excitable but not g
Usually possesses insight randiose/elated
Reports being unable to function
Reports high-level
Tends to lack insight function, not reflecting
behaviour
Reduced need for sleep
Difficulty getting off to sleep
Episodes of depression
Chronic low self-esteem
Reduced need for sleep tion, not reflecting
Reports high-level func
Difficulty getting off to sleep
Reports being unable to function
behaviour
Chronic low self-esteem
Complains
of
being
Episodes of depression sharpened mental
Usually possesses insight
Tends to lack insight
behaviour
Complains
of
Chronic low self-esteem
Episodes of depression
Usually possesses insight
Tends to lack insight
concentrate/focus
abilities
Difficulty getting of
Chronic low self-esteem
concentrate/focus f to sleep
Reduced need for sleep
Episodes of depression
abilities
Tends to lack insight
Usually possesses insight
Reduced need for sleep
Difficulty getting off to sleep
Restless (fidgety, difficulty being still)
Marked overactivity and agitation
being
to Subjective sense
unable
Tends to lack insight of sharpened mental
Usually possesses insight
Complains
of
Marked overactivity and agitation
Restless (fidgety, difficulty being still)
Reduced need for sleep
Difficulty getting off to sleep
unable
being
to Subjective sense of sharpened mental
Complains
of
Difficulty getting off to sleep
abilities
Source: Asherson, P being unable to Subjective sense of sharpened mental
concentrate/focus , Young AH, Eich-Höchli D et al. Differential diagnosis, comorbidity, and treatment
being
of
to Subjective sense of
unable
Reduced need for sleep sharpened mental
Complains
abilities
concentrate/focus
Source: Asherson, P, Young AH, Eich-Höchli D et al. Differential diagnosis, comorbidity, and treatment
being
of attention-deficit/hyperactivity disorder in relation to bipolar disorder or borderline personality
Complains dgety, difficulty being still) to Subjective sense of sharpened mental
Restless (fi
of
unable
Marked overactivity and agitation
abilities
concentrate/focus
of attention-deficit/hyperactivity disorder in relation to bipolar disorder or borderline personality
Marked overactivity and agitation
Restless (fidgety, difficulty being still)
disorder in adults. Current medical research and opinion. 2014;30(8):1657-1672
concentrate/focus
abilities
Restless (fidgety, difficulty being still)
Marked overactivity and agitation
disorder in adults. Current medical research and opinion. 2014;30(8):1657-1672
Source: Asherson, P, Young AH, Eich-Höchli D et al. Differential diagnosis, comorbidity, and treatment
Restless (fidgety, difficulty being still)
Source: Asherson, P, Young AH, Eich-Höchli D et al. Differential diagnosis, comorbidity, and treatment
Marked overactivity and agitation
of attention-deficit/hyperactivity disorder in relation to bipolar disorder or borderline personality
3.3. Co-Morbidities
Source: Asherson, P, Young AH, Eich-Höchli D et al. Differential diagnosis, comorbidity, and treatment
of attention-deficit/hyperactivity disorder in relation to bipolar disorder or borderline personality
3.3. Co-Morbidities
disorder in adults. Current medical research and opinion. 2014;30(8):1657-1672
of attention-deficit/hyperactivity disorder in relation to bipolar disorder or borderline personality
disorder in adults. Current medical research and opinion. 2014;30(8):1657-1672
Source: Asherson, P, Young AH, Eich-Höchli D et al. Differential diagnosis, comorbidity, and treatment
of attention-deficit/hyperactivity disorder in relation to bipolar disorder or borderline personality
BD pati ents may have psychiatric and medical co-morbidities. The co-morbidities cause
disorder in adults. Current medical research and opinion. 2014;30(8):1657-1672
BD patients may have psychiatric and medical co-morbidities. The co-morbidities cause
3.3. Co-Morbidities
disorder in adults. Current medical research and opinion. 2014;30(8):1657-1672
3.3. Co-Morbidities
difficulties in treatment e.g. decision on the drugs of choice and consideration of drug
difficulties in treatment e.g. decision on the drugs of choice and consideration of drug
3.3.
Co-Morbidities
interactions. It also affects the prognosis of BD in terms of aggravating the course of illness,
BD patients may have psychiatric and medical co-morbidities. The co-morbidities cause
interactions. It also affects the prognosis of BD in terms of aggravating the course of illness,
3.3. Co-Morbidities
BD patients may have psychiatric and medical co-morbidities. The co-morbidities cause
delaying recovery, increasing risk of recurrence and suicide, and reducing QoL.
difficulties in treatment e.g. decision on the drugs of choice and consideration of drug
delaying recovery, increasing risk of recurrence and suicide, and reducing QoL.
BD patients may have psychiatric and medical co-morbidities. The co-morbidities cause
difficulties in treatment e.g. decision on the drugs of choice and consideration of drug
interactions. It also affects the prognosis of BD in terms of aggravating the course of illness,
BD patients may have psychiatric and medical co-morbidities. The co-morbidities cause
difficulties in treatment e.g. decision on the drugs of choice and consideration of drug
23, level III
The prevalence of eating disorders in BD populations ranges from 1.9% to 33.3%.
23, level III The
interactions. It also affects the prognosis of BD in terms of aggravating the course of illness,
The
delaying recovery, increasing risk of recurrence and suicide, and reducing QoL.
The prevalence of eating disorders in BD populations ranges from 1.9% to 33.3%.
difficulties in treatment e.g. decision on the drugs of choice and consideration of drug
interactions. It also affects the prognosis of BD in terms of aggravating the course of illness,
prevalence of co-morbid antisocial personality disorder (ASPD) in BD ranges between 4.8%
delaying recovery, increasing risk of recurrence and suicide, and reducing QoL.
interactions. It also affects the prognosis of BD in terms of aggravating the course of illness,
prevalence of co-morbid antisocial personality disorder (ASPD) in BD ranges between 4.8%
delaying recovery, increasing risk of recurrence and suicide, and reducing QoL.
and 63%.It is higher in BD I (45.1%) than BD II (8.2%). The most commonly abused
The
23, level III
and 63%.It is higher in BD I (45.1%) than BD II (8.2%). The most commonly abused
The prevalence of eating disorders in BD populations ranges from 1.9% to 33.3%.
delaying recovery, increasing risk of recurrence and suicide, and reducing QoL.
23, level III
substances in BD with ASPD are a combination of cocaine and alcohol. People with this co-
The prevalence of eating disorders in BD populations ranges from 1.9% to 33.3%.
prevalence of co-morbid antisocial personality disorder (ASPD) in BD ranges between 4.8%
substances in BD with ASPD are a combination of cocaine and alcohol. People with this co-
The
The prevalence of eating disorders in BD populations ranges from 1.9% to 33.3%.
morbidity have early onset of symptoms, impulsive traits, increased episodes of depression
prevalence of co-morbid antisocial personality disorder (ASPD) in BD ranges between 4.8%
and 63%.It is higher in BD I (45.1%) than BD II (8.2%). The most commonly abused
The
23, level III
morbidity have early onset of symptoms, impulsive traits, increased episodes of depression
The prevalence of eating disorders in BD populations ranges from 1.9% to 33.3%.
prevalence of co-morbid antisocial personality disorder (ASPD) in BD ranges between 4.8%
24, level I most commonly abused
and 63%.It is higher in BD I (45.1%) than BD II (8.2%). The
and mania, aggressive behaviour and high suicide attempts.
substances in BD with ASPD are a combination of cocaine
and mania, aggressive behaviour and high suicide attempts.and alcohol. People with this co-
prevalence of co-morbid antisocial personality disorder (ASPD) in BD ranges between 4.8%
and 63%.It is higher in BD I (45.1%) than BD II (8.2%). The most commonly abused
substances in BD with ASPD are a combination of cocaine and alcohol. People with this co-
and 63%.It is higher in BD I (45.1%) than BD II (8.2%). The most commonly abused
morbidity have early onset of symptoms, impulsive traits, increased episodes of depression
substances in BD with ASPD are a combination of cocaine and alcohol. People with this co-
25, level II-2
Other psychiatric co-morbidities in BD include:
morbidity have early onset of symptoms, impulsive traits, increased episodes of depression
24, level I
Other psychiatric co-morbidities in BD include:cide attempts.
and mania, aggressive behaviour and high sui
substances in BD with ASPD are a combination of cocaine and alcohol. People with this co-
morbidity have early onset of symptoms, impulsive traits, increased episodes of depression
drug abuse (33.5%)
and mania, aggressive behaviour and high suicide attempts.
24, level I
drug abuse (33.5%)
morbidity have early onset of symptoms, impulsive traits, increased episodes of depression
24, level I
and mania, aggressive behaviour and high suicide attempts.
anxiety disorder (31.8%)
24, level I
anxiety disorder (31.8%)
25, level II-2
Other psychiatric co-morbidities in BD include: 25, level II-2 24, level I 23, level III The
and mania, aggressive behaviour and high suicide attempts.
borderline personality disorder (6.9%)
Other psychiatric co-morbidities in BD include:
25, level II-2
drug abuse (33.5%)
Other psychiatric co-morbidities in BD include:
borderline personality disorder (6.9%) 25, level II-2
ADHD (5.2%)
drug abuse (33.5%)
ADHD (5.2%)
anxiety disorder (31.8%)
Other psychiatric co-morbidities in BD include: 25, level II-2
drug abuse (33.5%)
anxiety disorder (31.8%)
borderline personality disorder (6.9%) 25, level II-2
drug abuse (33.5%)
anxiety disorder (31.8%)
borderline personality disorder (6.9%)
Patients with BD may have medical co-morbidities as follows: 25, level II-2
ADHD (5.2%)
Patients with BD may have medical co-morbidities as follows:
anxiety disorder (31.8%)
borderline personality disorder (6.9%)
ADHD (5.2%)
hypertension (31.1%)
hypertension (31.1%) disorder (6.9%)
borderline personality
asthma (11.7%)
ADHD (5.2%)
Patients with BD may have medical co-morbidities as follows: 25, level II-2
asthma (11.7%)
ADHD (5.2%)
Patients with BD may have medical co-morbidities as follows:
diabetes mellitus (11%)
25, level II-2
diabetes mellitus (11%)
hypertension (31.1%)
Patients with BD may have medical co-morbidities as follows: 25, level II-2
hypertension (31.1%)
obesity (11%)
asthma (11.7%)
obesity (11%)
Patients with BD may have medical co-morbidities as follows: 25, level II-2
hypothyroidism (11%)
asthma (11.7%)
hypertension (31.1%)
hypothyroidism (11%)
diabetes mellitus (11%)
hypertension (31.1%)
asthma (11.7%)
diabetes mellitus (11%)
migraine (5.5%)
obesity (11%)
asthma (11.7%)
migraine (5.5%)
diabetes mellitus (11%)
obesity (11%) is human immunodeficiency virus (HIV) infection (1%).
Another co-morbidity 26, level II-2
26, level II-2
Another co-morbidity is human immunodeficiency virus (HIV) infection (1%).
hypothyroidism (11%)
obesity (11%)
hypothyroidism (11%)
diabetes mellitus (11%)
migraine (5.5%)
obesity (11%)
hypothyroidism (11%)
migraine (5.5%)
Another co-morbidity is human immunodeficiency virus (HIV) infection (1%). 26, level II-2
hypothyroidism (11%)
migraine (5.5%)
Another co-morbidity is human immunodeficiency virus (HIV) infection (1%). 26, level II-2
migraine (5.5%)
Another co-morbidity is human immunodeficiency virus (HIV) infection (1%).
26, level II-2
26, level II-2
Another co-morbidity is human immunodeficiency virus (HIV) infection (1%).
5
5
5
5
5
5
5