Page 41 - e-book CPG - Bipolar Disorder
P. 41
CLINICAL PRACTICE GUIDELINES MANAGEMENT OF BIPOLAR DISORDER (2ND ED.)
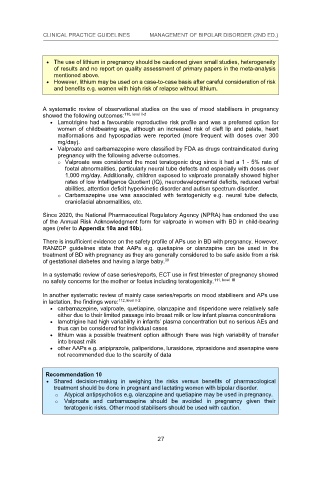
The use of lithium in pregnancy should be cautioned given small studies, heterogeneity
The use of lithium in pregnancy should be cautioned given small studies, heterogeneity
of results and no report on quality assessment of primary papers in the meta-analysis
The use of lithium in pregnancy should be cautioned given small studies, heterogeneity
of results and no report on quality assessment of primary papers in the meta-analysis
of results and no report on quality assessment of primary papers in the meta-analysis
mentioned above.
mentioned above.
However, lithium may be used on a case-to-case basis after careful consideration of risk
mentioned above.
However, lithium may be used on a case-to-case basis after careful consideration of risk
and benefits e.g. women with high risk of relapse without lithium.
However, lithium may be used on a case-to-case basis after careful consideration of risk
and benefits e.g. women with high risk of relapse without lithium.
and benefits e.g. women with high risk of relapse without lithium.
A systematic review of observational studies on the use of mood stabilisers in pregnancy
110, level II-2 studies on the use of mood stabilisers in pregnancy
A systematic review of observational
showed the following outcomes:
A systematic review of observational studies on the use of mood stabilisers in pregnancy
showed the following outcomes: 110, level II-2
110, level II-2
Lamotrigine had a favourable reproductive risk profile and was a preferred option for
showed the following outcomes:
Lamotrigine had a favourable reproductive risk profile and was a preferred option for
women of childbearing age, although an increased risk of cleft lip and palate, heart
Lamotrigine had a favourable reproductive risk profile and was a preferred option for
women of childbearing age, although an increased risk of cleft lip and palate, heart
malformations and hypospadias were reported (more frequent with doses over 300
women of childbearing age, although an increased risk of cleft lip and palate, heart
malformations and hypospadias were reported (more frequent with doses over 300
mg/day).
malformations and hypospadias were reported (more frequent with doses over 300
mg/day).
Valproate and carbamazepine were classified by FDA as drugs contraindicated during
mg/day).
Valproate and carbamazepine were classified by FDA as drugs contraindicated during
pregnancy with the following adverse outcomes.
Valproate and carbamazepine were classified by FDA as drugs contraindicated during
pregnancy with the following adverse outcomes.
o Valproate was considered the most teratogenic drug since it had a 1 - 5% rate of
pregnancy with the following adverse outcomes.
o Valproate was considered the most teratogenic drug since it had a 1 - 5% rate of
o Valproate was considered the most teratogenic drug since it had a 1 - 5% rate of
foetal abnormalities, particularly neural tube defects and especially with doses over
foetal abnormalities, particularly neural tube defects and especially with doses over
1,000 mg/day. Additionally, children exposed to valproate prenatally showed higher
foetal abnormalities, particularly neural tube defects and especially with doses over
1,000 mg/day. Additionally, children exposed to valproate prenatally showed higher
1,000 mg/day. Additionally, children exposed to valproate prenatally showed higher
rates of low Intelligence Quotient (IQ), neurodevelopmental deficits, reduced verbal
rates of low Intelligence Quotient (IQ), neurodevelopmental deficits, reduced verbal
rates of low Intelligence Quotient (IQ), neurodevelopmental deficits, reduced verbal
abilities, attention deficit hyperkinetic disorder and autism spectrum disorder.
abilities, attention deficit hyperkinetic disorder and autism spectrum disorder.
abilities, attention deficit hyperkinetic disorder and autism spectrum disorder. defects,
o Carbamazepine use was associated with teratogenicity e.g. neural tube
o Carbamazepine use was associated with teratogenicity e.g. neural tube defects,
o Carbamazepine use was associated with teratogenicity e.g. neural tube defects,
craniofacial abnormalities, etc.
craniofacial abnormalities, etc.
craniofacial abnormalities, etc.
Since 2020, the National Pharmaceutical Regulatory Agency (NPRA) has endorsed the use
Since 2020, the National Pharmaceutical Regulatory Agency (NPRA) has endorsed the use
Since 2020, the National Pharmaceutical Regulatory Agency (NPRA) has endorsed the use
of the Annual Risk Acknowledgment form for valproate in women with BD in child-bearing
of the Annual Risk Acknowledgment form for valproate in women with BD in child-bearing
ages (refer to Appendix 10a and 10b).
of the Annual Risk Acknowledgment form for valproate in women with BD in child-bearing
ages (refer to Appendix 10a and 10b).
ages (refer to Appendix 10a and 10b).
There is insufficient evidence on the safety profile of APs use in BD with pregnancy. However,
There is insufficient evidence on the safety profile of APs use in BD with pregnancy. However,
There is insufficient evidence on the safety profile of APs use in BD with pregnancy. However,
RANZCP guidelines state that AAPs e.g. quetiapine or olanzapine can be used in the
RANZCP guidelines state that AAPs e.g. quetiapine or olanzapine can be used in the
RANZCP guidelines state that AAPs e.g. quetiapine or olanzapine can be used in the
treatment of BD with pregnancy as they are generally considered to be safe aside from a risk
treatment of BD with pregnancy as they are generally considered to be safe aside from a risk
39
of gestational diabetes and having a large baby.
treatment of BD with pregnancy as they are generally considered to be safe aside from a risk
39
of gestational diabetes and having a large baby. 39
of gestational diabetes and having a large baby.
In a systematic review of case series/reports, ECT use in first trimester of pregnancy showed
In a systematic review of case series/reports, ECT use in first trimester of pregnancy showed
no safety concerns for the mother or foetus including teratogenicity.
111, level III
In a systematic review of case series/reports, ECT use in first trimester of pregnancy showed
111, level III
no safety concerns for the mother or foetus including teratogenicity. 111, level III
no safety concerns for the mother or foetus including teratogenicity.
In another systematic review of mainly case series/reports on mood stabilisers and APs use
In another systematic review of mainly case series/reports on mood stabilisers and APs use
112, level II-2
in lactation, the findings were:
In another systematic review of mainly case series/reports on mood stabilisers and APs use
112, level II-2
in lactation, the findings were: 112, level II-2
carbamazepine, valproate, quetiapine, olanzapine and risperidone were relatively safe
in lactation, the findings were:
carbamazepine, valproate, quetiapine, olanzapine and risperidone were relatively safe
either due to their limited passage into breast milk or low infant plasma concentrations
carbamazepine, valproate, quetiapine, olanzapine and risperidone were relatively safe
either due to their limited passage into breast milk or low infant plasma concentrations
lamotrigine had high variability in infants’ plasma concentration but no serious AEs and
either due to their limited passage into breast milk or low infant plasma concentrations
lamotrigine had high variability in infants’ plasma concentration but no serious AEs and
thus can be considered for individual cases
lamotrigine had high variability in infants’ plasma concentration but no serious AEs and
thus can be considered for individual cases
thus can be considered for individual cases
lithium was a possible treatment option although there was high variability of transfer
lithium was a possible treatment option although there was high variability of transfer
into breast milk
lithium was a possible treatment option although there was high variability of transfer
into breast milk
other AAPs e.g. aripiprazole, paliperidone, lurasidone, ziprasidone and asenapine were
into breast milk
other AAPs e.g. aripiprazole, paliperidone, lurasidone, ziprasidone and asenapine were
not recommended due to the scarcity of data
other AAPs e.g. aripiprazole, paliperidone, lurasidone, ziprasidone and asenapine were
not recommended due to the scarcity of data
not recommended due to the scarcity of data
Recommendation 10
Recommendation 10
Shared decision-m
Recommendation 10 aking in weighing the risks versus benefits of pharmacological
Shared decision-making in weighing the risks versus benefits of pharmacological
treatment should be done in pregnant and lactating women with bipolar disorder.
Shared decision-making in weighing the risks versus benefits of pharmacological
treatment should be done in pregnant and lactating women with bipolar disorder.
o Atypical antipsychotics e.g. olanzapine and quetiapine may be used in pregnancy.
treatment should be done in pregnant and lactating women with bipolar disorder.
o Atypical antipsychotics e.g. olanzapine and quetiapine may be used in pregnancy.
o Atypical antipsychotics e.g. olanzapine and quetiapine may be used in pregnancy.
o Valproate and carbamazepine should be avoided in pregnancy given their
o Valproate and carbamazepine should be avoided in pregnancy given their
teratogenic risks. Other mood stabilisers should be used with caution.
o Valproate and carbamazepine should be avoided in pregnancy given their
teratogenic risks. Other mood stabilisers should be used with caution.
teratogenic risks. Other mood stabilisers should be used with caution.
27
27
27
27