Page 46 - e-book CPG - Bipolar Disorder
P. 46
CLINICAL PRACTICE GUIDELINES MANAGEMENT OF BIPOLAR DISORDER (2ND ED.)
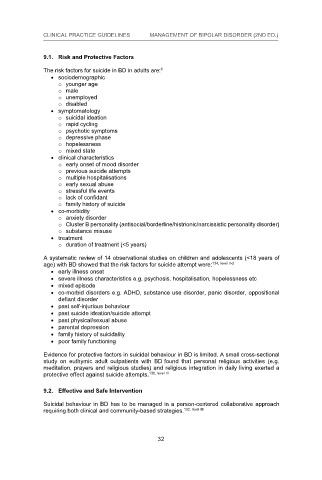
9.1. Risk and Protective Factors
9.1. Risk and Protective Factors
6
The risk factors for suicide in BD in adults are: 6
The risk factors for suicide in BD in adults are:
sociodemographic
sociodemographic
o younger age
o younger age
o male
o male
o unemployed
o unemployed
o disabled
o disabled
symptomatology
symptomatology
o suicidal ideation
o suicidal ideation
o rapid cycling
o rapid cycling
o psychotic symptoms
o psychotic symptoms
o depressive phase
o depressive phase
o hopelessness
o hopelessness
o mixed state
o mixed state
clinical characteristics
clinical characteristics
o early onset of mood disorder
o early onset of mood disorder
o previous suicide attempts
o previous suicide attempts
o multiple hospitalisations
o multiple hospitalisations
o early sexual abuse
o early sexual abuse
o stressful life events
o stressful life events
o lack of confidant
o lack of confidant
o family history of suicide
o family history of suicide
co-morbidity
co-morbidity
o anxiety disorder
o anxiety disorder
o Cluster B personality (antisocial/borderline/histrionic/narcissistic personality disorder)
o Cluster B personality (antisocial/borderline/histrionic/narcissistic personality disorder)
o substance misuse
o substance misuse
treatment
treatment
o duration of treatment (<5 years)
o duration of treatment (<5 years)
A systematic review of 14 observational studies on children and adolescents (<18 years of
A systematic review of 14 observational studies on children and adolescents (<18 years of
age) with BD showed that the risk factors for suicide attempt were: 134, level II-2
134, level II-2
age) with BD showed that the risk factors for suicide attempt were:
early illness onset
early illness onset
severe illness characteristics e.g. psychosis, hospitalisation, hopelessness etc
severe illness characteristics e.g. psychosis, hospitalisation, hopelessness etc
mixed episode
mixed episode
co-morbid disorders e.g. ADHD, substance use disorder, panic disorder, oppositional
co-morbid disorders e.g. ADHD, substance use disorder, panic disorder, oppositional
defiant disorder
defiant disorder
past self-injurious behaviour
past self-injurious behaviour
past suicide ideation/suicide attempt
past suicide ideation/suicide attempt
past physical/sexual abuse
past physical/sexual abuse
parental depression
parental depression
family history of suicidality
family history of suicidality
poor family functioning
poor family functioning
Evidence for protective factors in suicidal behaviour in BD is limited. A small cross-sectional
Evidence for protective factors in suicidal behaviour in BD is limited. A small cross-sectional
study on euthymic adult outpatients with BD found that personal religious activities (e.g.
study on euthymic adult outpatients with BD found that personal religious activities (e.g.
meditation, prayers and religious studies) and religious integration in daily living exerted a
meditation, prayers and religious studies) and religious integration in daily living exerted a
protective effect against suicide attempts. 136, level III
136, level III
protective effect against suicide attempts.
9.2. Effective and Safe Intervention
9.2. Effective and Safe Intervention
Suicidal behaviour in BD has to be managed in a person-centered collaborative approach
Suicidal behaviour in BD has to be managed in a person-centered collaborative approach
requiring both clinical and community-based strategies. 132, level III
132, level III
requiring both clinical and community-based strategies.
32
32
32