Page 3 - Vasoclick emagazine Issue2
P. 3
Vasoclick, Edition 2 02
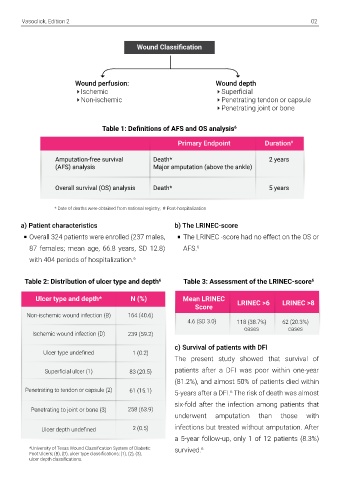
Wound Classification
Wound perfusion: Wound depth
Ischemic Superficial
Non-ischemic Penetrating tendon or capsule
Penetrating joint or bone
Table 1: Definitions of AFS and OS analysis 6
Primary Endpoint Duration # patients, however, AFS was significantly
Four major factors associated with a improved by revascularization in patients with
Amputation-free survival Death* 2 years 6
(AFS) analysis Major amputation (above the ankle) significantly shorter OS ischemic infection. Thus, timely management of
6
Major amputation(s) during hospitaliza- ischemic wound and early access to vascular
Overall survival (OS) analysis Death* 5 years tion (P<0.001; HR 6.673; CI surgery for limb salvage in diabetic patients is
2.836–15.700)
strongly recommended. 6
* Date of deaths were obtained from national registry; # Post-hospitalization
Wound ischemia: due to an infected
ulcer [(vs. non-ischemic wound; P=0.046;
a) Patient characteristics b) The LRINEC-score e) Infection
HR 1.598; CI 1.008–2.532)
Overall 324 patients were enrolled (237 males, The LRINEC -score had no effect on the OS or 1) Indicative of severe infection, high CRP
87 females; mean age, 66.8 years, SD 12.8) AFS. 6 Age: over 67 years (P<0.001; HR 1.055; levels were found to be associated with a
CI 1.035–1.076)
6
with 404 periods of hospitalization. 6 worse AFS.
Materials and methods The Laboratory Risk Indicator for Necrotizing Impaired renal functions: eGFR under 2) AFS was also associated with a deep wound
60 ml/min (P<0.001; HR 0.989; CI
The retrospective cohort study enrolled adult Fasciitis score (LRINEC score): Table 2: Distribution of ulcer type and depth 6 Table 3: Assessment of the LRINEC-score 6 0.982–0.995) (penetrating to the bone or joint) and high
patients presenting with acute DFI at the It is a sensitive scoring system to identify Ulcer type and depth* N (%) Mean LRINEC LRINEC >6 LRINEC >8 blood leukocytes. 6
Tampere University Hospital during 2010 necrotizing fasciitis and distinguish it from other Score Therefore, a diabetes patient presenting with an 3) Long-lasting and multiple foot ulcers were
8
-2014. 6,7 soft tissue infections. An LRINEC score of >8 Non-ischemic wound infection (B) 164 (40.6) 4.6 (SD 3.0) 118 (38.7%) 62 (20.3%) acute infection can undergo a minor amputation also associated with a worse outcome as
has been found to be sensitive for patients with Ischemic wound infection (D) 239 (59.2) cases cases to restrict the infection, and this way a major reported previously. 2, 6
Following patient-related information was diabetes. 9 c) Survival of patients with DFI amputation can be avoided, saving both limb and
collected from the hospital records: Ulcer type undefined 1 (0.2) The present study showed that survival of life of the patient. The study therefore emphasized on the
Patient demographics (age and gender) The present study assessed the utility of LRINEC patients after a DFI was poor within one-year importance of early detection and treatment of
Registered diagnoses (ischemic heart disease, score to diagnose severe DFI and a poor Superficial ulcer (1) 83 (20.5) (81.2%), and almost 50% of patients died within d) Effect of revascularization the infection for diabetic foot ulcers. 6
chronic obstructive pulmonary disease, con- prognosis. LRINEC score with a cutoff of >8 was Penetrating to tendon or capsule (2) 61 (15.1) 5-years after a DFI. The risk of death was almost The AFS was greatly reduced in patients with
6
gestive heart failure and dyslipidemia, microbi- chosen to identify necrotizing fasciitis. 6 six-fold after the infection among patients that ischemic wounds. 16.1% of the cases had f) Hypertension
ological and clinical chemistry findings, surgi- Penetrating to joint or bone (3) 258 (63.9) underwent amputation than those with revascularization within 1 month of admission The study demonstrated that use of a
cal revisions and amputations, open and endo- A specialist in plastic surgery staged the wounds 2 (0.5) infections but treated without amputation. After and in most cases within 1 week. 6 hypertensive medication was associated with an
vascular revascularization procedures, wound according to the University of Texas Staging Ulcer depth undefined a 5-year follow-up, only 1 of 12 patients (8.3%) increased AFS, however the observation requires
status, and the length of hospital stay). 6 System for Diabetic Foot Ulcers (UT scale). 6,10 *University of Texas Wound Classification System of Diabetic survived. 6 Revascularization procedure (open or further validation. 6
Foot Ulcers; (B), (D), ulcer type classifications; (1), (2), (3),
ulcer depth classifications. endovascular) had no effect on survival of
Conclusion 7) LaaksoM, Kiiski J, KarppelinM, HelminenM, Kaartinen I.
Pathogens causing diabetic foot infection and the
Patients with DFI have high morbidity and reliability of the superficial culture. Surg Infect. 2020. doi:
poor survival outcomes despite advanced 10.1089/sur.2020.072.
treatment resources. 8) Wong C-H, Khin L-W, Heng K-S, Tan K-C, Low C-O. The
6
LRINEC (Laboratory Risk Indicator for Necrotizing
High CRP levels are associated with a Fasciitis) score: a tool for distinguishing necrotizing
reduced AFS. fasciitis from other soft tissue infections. Crit Care Med.
6
2004; 32:1535–41. doi:
Ischemic infections in deep wounds with 10.1097/01.CCM.0000129486.35458.7D
high CRP levels suggest severity of the 9)Tan JH, Koh BTH, Hong CC, Lim SH, Liang S, Chan GEH,
disease and must be prevented early. 6 et al. A comparison of necrotising fasciitis in diabetics
and non-diabetics: a review of 127 patients. Bone Joint J.
A major amputation is a strong predictor of (2016) 98-B:1563–8. doi:
10.1302/0301-620X.98B11.37526
death in patients with DFI.
6
Thus, early identification and treatments of 10) Lavery LA, Armstrong DG, Harkless LB. Classification
of diabetic foot wounds. J Foot Ankle Surg. 1996; 35:528–
DFI are critical to improve both the AFS and 31. doi: 10.1016/S1067-2516(96)80125-6
OS.
6
References:
1) Armstrong DG, Swerdlow MA, Armstrong AA, Conte MS,
Padula WV, Bus SA. Five year mortality and direct costs of
care for people with diabetic foot complications are
comparable to cancer. J Foot Ankle Res. 2020;13:16. doi:
10.1186/s13047-020-00383-2
2) Ndosi M, Wright-Hughes A, Brown S, Backhouse M,
Lipsky BA, Bhogal M, et al. Prognosis of the infected
diabetic foot ulcer: a 12-month prospective observational
study. Diabet Med. 2018; 35:78–88. doi:
10.1111/dme.13537
3) Huang Y-Y, Lin C-W, Yang H-M, Hung S-Y, Chen I-W.
Survival and associated risk factors in patients with
diabetes and amputations caused by infectious foot
gangrene. J Foot Ankle Res. 2018; 11:1. doi:
10.1186/s13047-017-0243-0
4) Raspovic KM, Wukich DK. Self-reported quality of life
and diabetic foot infections. J Foot Ankle Surg. 2014;
53:716–9. doi: 10.1053/j.jfas.2014.06.011
5) Peters EJ, Childs MR, Wunderlich RP, Harkless LB,
Armstrong DG, Lavery LA. Functional status of persons
with diabetesrelated lower-extremity amputations.
Diabetes Care. 2000; 24:1799-804. doi:
10.2337/diacare.24.10.1799
6) Vuorlaakso M, Kiiski J, Salonen T, Karppelin M,
Helminen M, Kaartinen I. Major Amputation Profoundly
Increases Mortality in Patients With Diabetic Foot
Infection. Front Surg. 2021;8:655902. Published 2021 Apr
30.doi:10.3389/fsurg.2021.655902