Page 9 - CASA Bulletin of Anesthesiology 2022; 9(3)-1 (1)
P. 9
Vol. 9, No 3, 2022
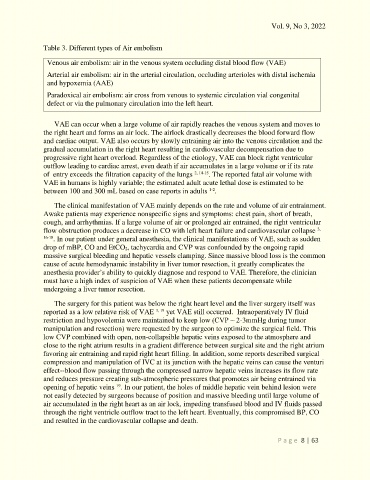
Table 3. Different types of Air embolism
Venous air embolism: air in the venous system occluding distal blood flow (VAE)
Arterial air embolism: air in the arterial circulation, occluding arterioles with distal ischemia
and hypoxemia (AAE)
Paradoxical air embolism: air cross from venous to systemic circulation vial congenital
defect or via the pulmonary circulation into the left heart.
VAE can occur when a large volume of air rapidly reaches the venous system and moves to
the right heart and forms an air lock. The airlock drastically decreases the blood forward flow
and cardiac output. VAE also occurs by slowly entraining air into the venous circulation and the
gradual accumulation in the right heart resulting in cardiovascular decompensation due to
progressive right heart overload. Regardless of the etiology, VAE can block right ventricular
outflow leading to cardiac arrest, even death if air accumulates in a large volume or if its rate
of entry exceeds the filtration capacity of the lungs 2, 14-15 . The reported fatal air volume with
VAE in humans is highly variable; the estimated adult acute lethal dose is estimated to be
between 100 and 300 mL based on case reports in adults .
1-2
The clinical manifestation of VAE mainly depends on the rate and volume of air entrainment.
Awake patients may experience nonspecific signs and symptoms: chest pain, short of breath,
cough, and arrhythmias. If a large volume of air or prolonged air entrained, the right ventricular
flow obstruction produces a decrease in CO with left heart failure and cardiovascular collapse 3,
16-18 . In our patient under general anesthesia, the clinical manifestations of VAE, such as sudden
drop of mBP, CO and EtCO2, tachycardia and CVP was confounded by the ongoing rapid
massive surgical bleeding and hepatic vessels clamping. Since massive blood loss is the common
cause of acute hemodynamic instability in liver tumor resection, it greatly complicates the
anesthesia provider’s ability to quickly diagnose and respond to VAE. Therefore, the clinician
must have a high index of suspicion of VAE when these patients decompensate while
undergoing a liver tumor resection.
The surgery for this patient was below the right heart level and the liver surgery itself was
reported as a low relative risk of VAE 3, 19 yet VAE still occurred. Intraoperatively IV fluid
restriction and hypovolemia were maintained to keep low (CVP ⁓ 2-3mmHg during tumor
manipulation and resection) were requested by the surgeon to optimize the surgical field. This
low CVP combined with open, non-collapsible hepatic veins exposed to the atmosphere and
close to the right atrium results in a gradient difference between surgical site and the right atrium
favoring air entraining and rapid right heart filling. In addition, some reports described surgical
compression and manipulation of IVC at its junction with the hepatic veins can cause the venturi
effect--blood flow passing through the compressed narrow hepatic veins increases its flow rate
and reduces pressure creating sub-atmospheric pressures that promotes air being entrained via
19
opening of hepatic veins . In our patient, the holes of middle hepatic vein behind lesion were
not easily detected by surgeons because of position and massive bleeding until large volume of
air accumulated in the right heart as an air lock, impeding transfused blood and IV fluids passed
through the right ventricle outflow tract to the left heart. Eventually, this compromised BP, CO
and resulted in the cardiovascular collapse and death.
P a g e 8 | 63