Page 10 - Hospitalists - Risks When You're the Doctor in the House (Part Two)
P. 10
SVMIC Hospitalists - Risks When You’re the Doctor in the House
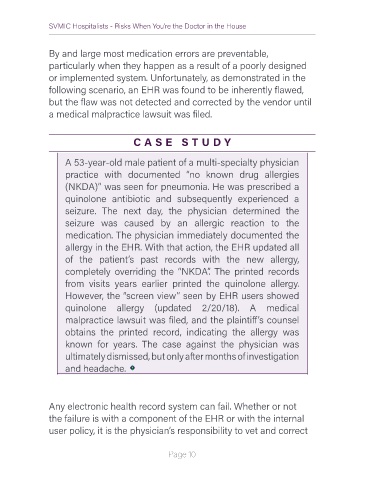
By and large most medication errors are preventable,
particularly when they happen as a result of a poorly designed
or implemented system. Unfortunately, as demonstrated in the
following scenario, an EHR was found to be inherently flawed,
but the flaw was not detected and corrected by the vendor until
a medical malpractice lawsuit was filed.
C A S E S T U DY
A 53-year-old male patient of a multi-specialty physician
practice with documented “no known drug allergies
(NKDA)” was seen for pneumonia. He was prescribed a
quinolone antibiotic and subsequently experienced a
seizure. The next day, the physician determined the
seizure was caused by an allergic reaction to the
medication. The physician immediately documented the
allergy in the EHR. With that action, the EHR updated all
of the patient’s past records with the new allergy,
completely overriding the “NKDA”. The printed records
from visits years earlier printed the quinolone allergy.
However, the “screen view” seen by EHR users showed
quinolone allergy (updated 2/20/18). A medical
malpractice lawsuit was filed, and the plaintiff’s counsel
obtains the printed record, indicating the allergy was
known for years. The case against the physician was
ultimately dismissed, but only after months of investigation
and headache.
Any electronic health record system can fail. Whether or not
the failure is with a component of the EHR or with the internal
user policy, it is the physician’s responsibility to vet and correct
Page 10