Page 191 - Demonstrating skill coppysaved colored-converted
P. 191
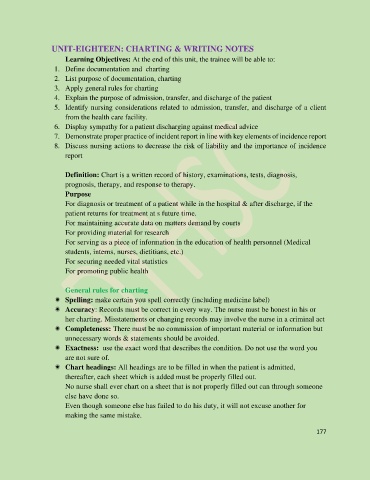
UNIT-EIGHTEEN: CHARTING & WRITING NOTES
Learning Objectives: At the end of this unit, the trainee will be able to:
1. Define documentation and charting
2. List purpose of documentation, charting
3. Apply general rules for charting
4. Explain the purpose of admission, transfer, and discharge of the patient
5. Identify nursing considerations related to admission, transfer, and discharge of a client
from the health care facility.
6. Display sympathy for a patient discharging against medical advice
7. Demonstrate proper practice of incident report in line with key elements of incidence report
8. Discuss nursing actions to decrease the risk of liability and the importance of incidence
report
Definition: Chart is a written record of history, examinations, tests, diagnosis,
prognosis, therapy, and response to therapy.
Purpose
For diagnosis or treatment of a patient while in the hospital & after discharge, if the
patient returns for treatment at s future time.
For maintaining accurate data on matters demand by courts
For providing material for research
For serving as a piece of information in the education of health personnel (Medical
students, interns, nurses, dietitians, etc.)
For securing needed vital statistics
For promoting public health
General rules for charting
Spelling: make certain you spell correctly (including medicine label)
Accuracy: Records must be correct in every way. The nurse must be honest in his or
her charting. Misstatements or changing records may involve the nurse in a criminal act
Completeness: There must be no commission of important material or information but
unnecessary words & statements should be avoided.
Exactness: use the exact word that describes the condition. Do not use the word you
are not sure of.
Chart headings: All headings are to be filled in when the patient is admitted,
thereafter, each sheet which is added must be properly filled out.
No nurse shall ever chart on a sheet that is not properly filled out can through someone
else have done so.
Even though someone else has failed to do his duty, it will not excuse another for
making the same mistake.
177