Page 4 - PWH.19 Employee Benefits
P. 4
About the HIP Plan Benefit
Offered by Positrol, Inc
Effective January 2016
Your employer, Positrol, Inc, is sponsoring a HIP Plan that works like secondary insurance coverage to help cover
certain expenses not covered by your primary insurance with ANTHEM. Custom Design Benefits administers the
program.
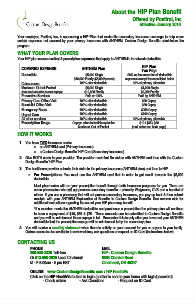
WHAT YOUR PLAN COVERS
Your HIP plan covers medical & prescription expenses that apply to ANTHEM’s in-network deductible.
COVERED EXPENSE ANTHEM Plan HIP Plan
You Pay:
Deductible $5,000 Single
$10,000 Family ($5,000/person) 20% co-insurance for all deductible
Coinsurance expenses except the ones listed below
Maximum Out-of-Pocket 100% after deductible
$5,000 Single 20% of primary allowable
(includes Deductible but not copays) $10,000 Family $1,000 Single
Paid at 100% $2,000 Family
Preventive Services
Primary Care Office Visit 100% after deductible Paid by ANTHEM
Specialist Office Visit 100% after deductible
Emergency Room 100% after deductible $30 Copay
Urgent Care 100% after deductible
All other services 100% after deductible $60 Copay
Prescription Drugs Copays after deductible up to the
Maximum Out-of-Pocket $250 Copay
$100 Copay
20% of primary allowable
$10 / $35 / $60
(mail order-see back page)
HOW IT WORKS
1. You have TWO insurance cards:
o an ANTHEM card (Primary insurance)
o a Custom Design Benefits’ HIP Card (Secondary insurance)
2. Give BOTH cards to your provider. The provider must first file claims with ANTHEM and then with the Custom
Design Benefits’ HIP Plan.
3. The healthcare provider submits their claim to the primary insurance (ANTHEM plan) and then to HIP.
o For Prescriptions: You must use the ANTHEM card first in order to get credit towards the $5,000
deductible.
Most pharmacies will run your prescription benefit through both insurance programs for you. There are
some pharmacies who will not process secondary benefits – primarily Walgreens, CVS and a handful of
others. If you use a pharmacy that will not process secondary insurance, you pay up front & then submit
receipts with your ANTHEM Explanation of Benefits to Custom Design Benefits. See reverse side for
additional instructions regarding the use of your HIP pharmacy benefit.
*If a member meets the ANTHEM deductible and purchases a prescription the primary plan will continue
to have a copayment of $10, $35 & $70. These amounts can be submitted to Custom Design Benefits
and you will be reimbursed those copays in full. Remember this is only after you have met your ANTHEM
deductible that the prescription copays will be reimbursed to by the secondary plan.
4. You will receive a monthly statement when there is activity on your account for you or anyone in your family.
Online access is also available to review claims, ask questions or request an ID Card (instructions below).
CONTACTING US MAIL
HIP - Custom Design Benefits
PHONE 5589 Cheviot Road
800-598-2929 Toll-free Cincinnati, OH 45247
Or 513-598-2929 Local Cincinnati
M - F 8:00am - 5 pm EST
ONLINE www.CustomDesignBenefits.com / HIP HealthVu
Click on the HIP HealthVu button to login (a letter is sent to your home with login/password)
- Check claims - Ask Questions - Request an ID Card