Page 7 - QR-SLE-8_5_24
P. 7
T
OF SYSTEMIC LUPUS ER
MANAGEMENT
YTHEMA
YTHEMA
T
QUICK REFERENCE FOR HEAL
MANAGEMENT
QUICK REFERENCE FOR HEAL
OF SYSTEMIC LUPUS ER
QUICK REFERENCE FOR HEALTHCARE PROVIDERSTHCARE PROVIDERS MANAGEMENT OF SYSTEMIC LUPUS ERYTHEMATOSUSOSUS QUICK REFERENCE FOR HEALTHCARE PROVIDERSTHCARE PROVIDERS MANAGEMENT OF SYSTEMIC LUPUS ERYTHEMATOSUSOSUS
CLINICAL MANIFESTATIONS
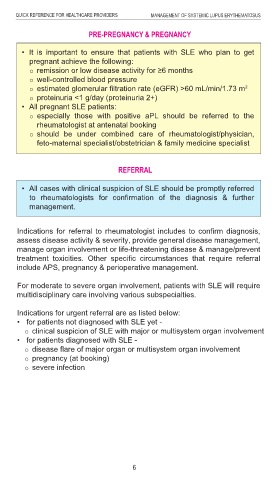
TREATMENT PRE-PREGNANCY & PREGNANCY
KEY MESSAGES
1. Systemic lupus erythematosus (SLE) is a chronic autoimmune
• Principles of SLE treatment are to achieve: • It is important to ensure that patients with SLE who plan to get
Neuropsychiatry
multisystem disorder with diverse & complex clinical manifestations
disease remission pregnant achieve the following: • Polyneuropathy • Acute confusion state
characterised by inflammation in a variety of organs. It has a remission or low disease activity for ≥6 months
• Cerebrovascular • Headache/Migraine
disease flare prevention
relapsing-remitting course with a very unpredictable prognosis & disease/Stroke • Transverse myelitis
organ damage prevention well-controlled blood pressure
considerable morbidity. • Seizure • Cognitive impairment
quality of life improvement
estimated glomerular filtration rate (eGFR) >60 mL/min/1.73 m
2
2. Diagnosis of SLE should be based on clinical manifestations Mucocutaneous • Psychosis
minimisation of drug side-effects • Malar rash
proteinuria <1 g/day (proteinuria 2+)
supported by laboratory findings following exclusion of alternative
• If complete remission cannot be achieved, the lowest possible • All pregnant SLE patients: Eye
• Oral ulcers
diagnoses. • Photosensitivity • Dry eyes
disease activity in all organs involved should be targeted.
especially those with positive aPL should be referred to the
3. All patients with SLE should have clinical assessments of disease • Discoid rash • Retinal vasculitis
rheumatologist at antenatal booking
activity using validated assessment tools. • Alopecia • Optic neuritis
should be under combined care of rheumatologist/physician,
4. Patients with SLE should practise sun avoidance &, use protective Cardio-respiratory
FREQUENCY & PARAMETERS FOR MONITORING
feto-maternal specialist/obstetrician & family medicine specialist
clothing & broad-spectrum sunscreen with at least sun protection • ILD Haematology
factor (SPF) 50. Patients with Patients with stable/ • Pericarditis • Leukopenia
active disease
5. Corticosteroids should be used for acute flare in SLE; the dose should • PAH • Thrombocytopenia
low disease activity
At first
• AIHA
Assessments visit should be reviewed should be reviewed • Pleurisy REFERRAL • Lymphopenia
be minimised accordingly & discontinued whenever possible.
• Serositis
at least every
6. All patients with SLE should be on hydroxychloroquine (HCQ) unless • Myocarditis • APS
every 6 - 12 months
• All cases with clinical suspicion of SLE should be promptly referred
intolerant or contraindicated. 1 - 3 months • Libman-Sacks
to
Clinical
7. Immunosuppressants should be considered as add-on therapy to endocarditis rheumatologists for confirmation of the diagnosis & further
management.
History Renal Gastrointestinal
patients with SLE not responding to HCQ alone or in combination with
Vital signs • Proteinuria • Pancreatitis
corticosteroids, or when corticosteroids doses cannot be tapered.
Clinical examination
• Microscopic
8. Infection in patients with SLE should be identified early & treated Indications • Enteritis
haematuriafor referral to rheumatologist includes to confirm diagnosis,
• Lupoid hepatitis
Drug review assess disease activity & severity, provide general disease management,
accordingly.
Blood tests
9. All women with SLE in the reproductive age group should receive manage organ involvement or life-threatening disease & manage/prevent
FBC treatment toxicities. Other specific circumstances that require referral
• Raynaud’s
pre-pregnancy counselling.
RP
10. In SLE with pregnancy, HCQ, azathioprine, calcineurin inhibitors & low include APS, pregnancy & perioperative management. phenomenon
Vasculitis
LFT
dose corticosteroids should be continued.
CRP a a
Musculoskeletal
ESR This Quick Reference provides key messages & summarises the main For moderate to severe organ involvement, patients with SLE will require
• Arthritis/Arthralgia
multidisciplinary care involving various subspecialties.
Bone profile a a a Constitutional • Myositis
recommendations in the Clinical Practice Guidelines (CPG) Management of Systemic
-
Vitamin D3 Lupus Erythematosus. a symptoms
a
• Fever
Immunology/serology Indications for urgent referral are as listed below:
• Fatigue
ANA Details of the evidence supporting these recommendations can be found in the • for patients not diagnosed with SLE yet -
-
• Weight loss
-
clinical suspicion of SLE with major or multisystem organ involvement
Anti-dsDNA above CPG, available on the following websites: a • for patients diagnosed with SLE -
a
C3/C4 levels Ministry of Health Malaysia: www.moh.gov.my a disease flare of major organ or multisystem organ involvement
a
aPL Academy of Medicine Malaysia: www.acadmed.org.my a,p pregnancy (at booking)
a
ENA Malaysian Society of Rheumatology: msr.my a,p severe infection
a
Immunoglobulin A, G, M a a a AIHA = autoimmune haemolytic anaemia; APS = antiphospholipid syndrome; ILD =
CLINICAL PRACTICE GUIDELINES SECRETARIAT
Direct Coombs’ test a a interstitial lung disease; PAH = pulmonary arterial hypertension
Malaysian Health Technology Assessment Section (MaHTAS)
Urine Medical Development Division, Ministry of Health Malaysia
UFEME Level 4, Block E1, Precinct 1,
Urine random protein:
Federal Government Administrative Centre
creatinine ratio OR 62590 Putrajaya, Malaysia a
a
a
24-hour urine protein Tel: 603-88831229
E-mail: htamalaysia@moh.gov.my
= indicated; = when indicated; = when indicated during pregnancy; - = not
a
a,p
indicated; anti-dsDNA = anti-double stranded deoxyribonucleic acid; ENA = extractable
nuclear antigen
51 26