Page 255 - IC38 GENERAL INSURANCE
P. 255
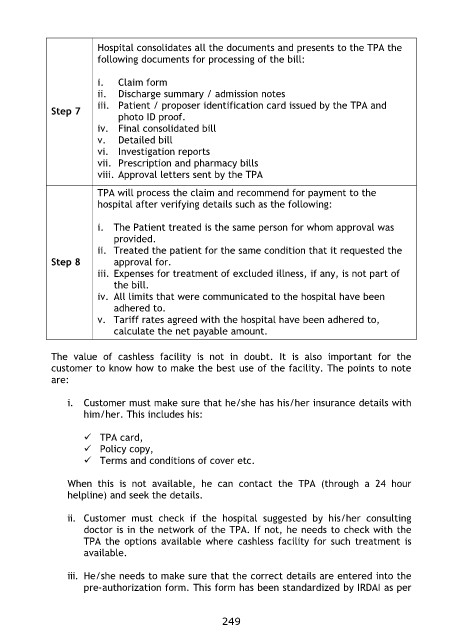
Hospital consolidates all the documents and presents to the TPA the
following documents for processing of the bill:
Step 7 i. Claim form
Step 8 ii. Discharge summary / admission notes
iii. Patient / proposer identification card issued by the TPA and
photo ID proof.
iv. Final consolidated bill
v. Detailed bill
vi. Investigation reports
vii. Prescription and pharmacy bills
viii. Approval letters sent by the TPA
TPA will process the claim and recommend for payment to the
hospital after verifying details such as the following:
i. The Patient treated is the same person for whom approval was
provided.
ii. Treated the patient for the same condition that it requested the
approval for.
iii. Expenses for treatment of excluded illness, if any, is not part of
the bill.
iv. All limits that were communicated to the hospital have been
adhered to.
v. Tariff rates agreed with the hospital have been adhered to,
calculate the net payable amount.
The value of cashless facility is not in doubt. It is also important for the
customer to know how to make the best use of the facility. The points to note
are:
i. Customer must make sure that he/she has his/her insurance details with
him/her. This includes his:
TPA card,
Policy copy,
Terms and conditions of cover etc.
When this is not available, he can contact the TPA (through a 24 hour
helpline) and seek the details.
ii. Customer must check if the hospital suggested by his/her consulting
doctor is in the network of the TPA. If not, he needs to check with the
TPA the options available where cashless facility for such treatment is
available.
iii. He/she needs to make sure that the correct details are entered into the
pre-authorization form. This form has been standardized by IRDAI as per
249