Page 117 - Trident 2022 Flipbook
P. 117
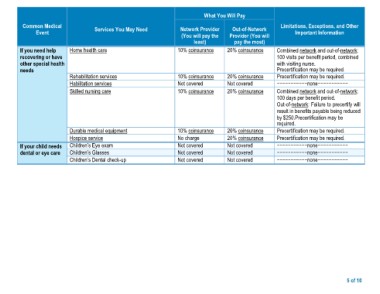
What You Will Pay
Common Medical Services You May Need Network Provider Out-of-Network Limitations, Exceptions, and Other
Event (You will pay the Provider (You will Important Information
If you need help Home health care least) pay the most) Combined network and out-of-network:
recovering or have 100 visits per benefit period, combined
other special health Rehabilitation services 10% coinsurance 20% coinsurance with visiting nurse.
needs Habilitation services Precertification may be required.
Skilled nursing care Precertification may be required.
10% coinsurance 20% coinsurance −−−−−−−−−−−none−−−−−−−−−−−
Not covered Not covered Combined network and out-of-network:
10% coinsurance 20% coinsurance 100 days per benefit period.
Out-of-network: Failure to precertify will
If your child needs Durable medical equipment 10% coinsurance 20% coinsurance result in benefits payable being reduced
dental or eye care Hospice service No charge 20% coinsurance by $250.Precertification may be
Children’s Eye exam Not covered Not covered required.
Children’s Glasses Not covered Not covered Precertification may be required.
Children’s Dental check-up Not covered Not covered Precertification may be required.
−−−−−−−−−−−none−−−−−−−−−−−
−−−−−−−−−−−none−−−−−−−−−−−
−−−−−−−−−−−none−−−−−−−−−−−
5 of 10