Page 12 - Trident 2022 Flipbook
P. 12
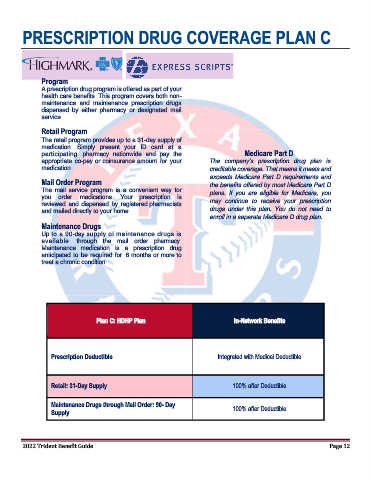
PRESCRIPTION DRUG COVERAGE PLAN C
Program
A prescription drug program is offered as part of your
health care benefits. This program covers both non-
maintenance and maintenance prescription drugs
dispensed by either pharmacy or designated mail
service
Retail Program
The retail program provides up to a 31-day supply of
medication. Simply present your ID card at a
participating pharmacy nationwide and pay the Medicare Part D
appropriate co-pay or coinsurance amount for your The company’s prescription drug plan is
medication. creditable coverage. That means it meets and
exceeds Medicare Part D requirements and
Mail Order Program the benefits offered by most Medicare Part D
The mail service program is a convenient way for plans. If you are eligible for Medicare, you
you order medications. Your prescription is may continue to receive your prescription
reviewed and dispensed by registered pharmacists
and mailed directly to your home. drugs under this plan. You do not need to
enroll in a separate Medicare D drug plan.
Maintenance Drugs
Up to a 90-day supply of maintenance drugs is
available through the mail order pharmacy.
Maintenance medication is a prescription drug
anticipated to be required for 6 months or more to
treat a chronic condition.
Plan C: HDHP Plan In-Network Benefits
Prescription Deductible Integrated with Medical Deductible
Retail: 31-Day Supply 100% after Deductible
Maintenance Drugs through Mail Order: 90- Day 100% after Deductible
Supply
2022 Trident Benefit Guide Page 12