Page 95 - Trident 2022 Flipbook
P. 95
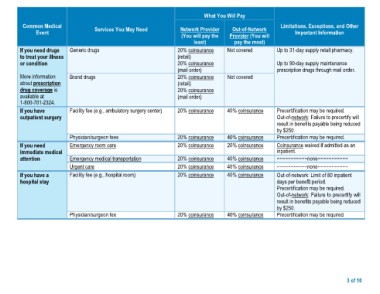
What You Will Pay
Common Medical Services You May Need Network Provider Out-of-Network Limitations, Exceptions, and Other
Event (You will pay the Provider (You will Important Information
If you need drugs Generic drugs least) pay the most) Up to 31-day supply retail pharmacy.
to treat your illness Not covered
or condition 20% coinsurance Up to 90-day supply maintenance
(retail) Not covered prescription drugs through mail order.
20% coinsurance
More information Brand drugs (mail order)
about prescription Facility fee (e.g., ambulatory surgery center)
drug coverage is 20% coinsurance
available at (retail)
1-800-701-2324. 20% coinsurance
(mail order)
If you have
outpatient surgery 20% coinsurance 40% coinsurance Precertification may be required.
Out-of-network: Failure to precertify will
If you need Physician/surgeon fees 20% coinsurance 40% coinsurance result in benefits payable being reduced
immediate medical Emergency room care 20% coinsurance 20% coinsurance by $250.
attention 20% coinsurance 40% coinsurance Precertification may be required.
Emergency medical transportation 20% coinsurance 40% coinsurance
If you have a Urgent care 20% coinsurance 40% coinsurance Coinsurance waived if admitted as an
hospital stay Facility fee (e.g., hospital room) inpatient.
20% coinsurance 40% coinsurance
Physician/surgeon fee −−−−−−−−−−−none−−−−−−−−−−−
−−−−−−−−−−−none−−−−−−−−−−−
Out-of-network: Limit of 80 inpatient
days per benefit period.
Precertification may be required.
Out-of-network: Failure to precertify will
result in benefits payable being reduced
by $250.
Precertification may be required.
3 of 10