Page 96 - Trident 2022 Flipbook
P. 96
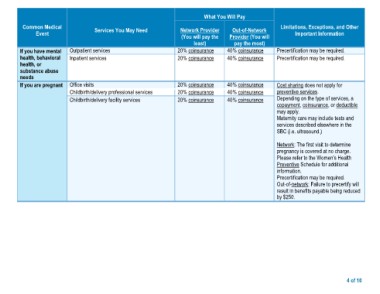
What You Will Pay
Common Medical Services You May Need Network Provider Out-of-Network Limitations, Exceptions, and Other
Event (You will pay the Provider (You will Important Information
If you have mental Outpatient services least) pay the most) Precertification may be required.
health, behavioral Inpatient services 20% coinsurance 40% coinsurance Precertification may be required.
health, or
substance abuse Office visits 20% coinsurance 40% coinsurance
needs Childbirth/delivery professional services
Childbirth/delivery facility services 20% coinsurance 40% coinsurance Cost sharing does not apply for
If you are pregnant 20% coinsurance 40% coinsurance preventive services.
20% coinsurance 40% coinsurance Depending on the type of services, a
copayment, coinsurance, or deductible
may apply.
Maternity care may include tests and
services described elsewhere in the
SBC (i.e. ultrasound.)
Network: The first visit to determine
pregnancy is covered at no charge.
Please refer to the Women’s Health
Preventive Schedule for additional
information.
Precertification may be required.
Out-of-network: Failure to precertify will
result in benefits payable being reduced
by $250.
4 of 10