Page 7 - SPRING 2016
P. 7
tage, medication or rinses were used after the extraction. DISCUSSION
Osteotomy was done with normal drilling protocols and a Implants can successfully integrate in infected sites following sur-
3.5/11mm implant was directed palatally to achieve good pri- gical, prosthetic, and periodontal principles. When implants are
mary stability and an implant stability quotient (ISQ) of 70. No stabilized at initial placement without filling the gap distance, and
graft or filler was used to close the gap distance measuring 4mm the provisional restoration is not in occlusion, we are able to
(Figure 4). A passively seated provisional was fabricated to pro- enhance the regenerative process from the periosteal cells by sup-
vide tertiary closure to the site. The provisional was designed to porting and maintaining space, which is critical during and after
provide support and form to the peri-implant tissue, and the crown the healing process. Therefore, recommendations are made to
margins were extended subgingivally by 3mm, providing neces- leave a gap distance of 3-4 mm and then maintain this gap during
sary support to the facial tissue as well as maintaining space for the entire healing process with the help of the provisional restora-
tissue regeneration (Figure 5). During a six month follow-up, we tion. Initial resorption is inevitable and will occur even with the
achieved osseointegration of the implant and the soft tissue con- best techniques and, therefore, the goal should be to reduce surgi-
tours were maintained with the help of the provisional restoration cal trauma as much as possible and to not disturb the surrounding
(Figure 6). In addition, we had improved ISQ values; there was an tissue during the surgical phase. Reflecting tissue should be avoid-
overall bucco-lingual tissue width reduction of 17% with 20% ed whenever possible during immediate placement because it
reduction in total bone volume. However, we gained facial plate causes more trauma, inflammation, and shrinkage. This case study
height and an increase in the facial plate thickness by over 70%; demonstrates and supports the principles discussed earlier in this
ending facial bone thickness being 2.85mm from 0.53mm. article about natural healing of sites and about leaving enough bio-
(Figure 7). Soft tissue at the time of cementation was in line with logic space and supporting tissue to allow for natural bone and tis-
the contours of the contralateral side (Fig 8). During the routine sue regeneration.
follow-up visit at one year from surgery, the soft tissue contours
were maintained (Figures 9, 10).
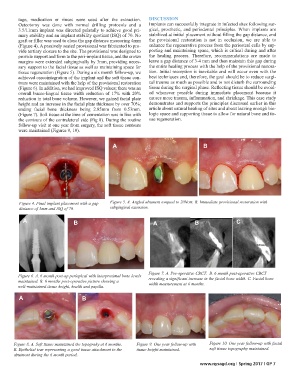
A B
Figure 4. Final implant placement with a gap Figure 5. A. Angled abument torqued to 20Ncm. B. Immediate provisional restoration with
distance of 3mm and ISQ of 70. subgingival extension.
A B A B C
Figure 7. A. Pre-operative CBCT. B. 6 month post-operative CBCT
Figure 6. A. 6 month post-op periapical with interproximal bone levels
maintained. B. 6 months post-operative picture showing a revealing a significant increase in the facial bone width. C. Facial bone
well-maintained tissue height, health and papilla. width measurement at 6 months.
A B
Figure 8. A. Soft tissue maintained the topograhy at 6 months. Figure 9. One year follow-up with Figure 10. One year follow-up with facial
B. Epithelial tear representing a good tissue attachment to the tissue height maintained. soft tissue topography maintained.
abutment during the 6 month period.
www.nysagd.org | Spring 2017 | GP 7