Page 3 - Forms - New Patient Paperwork (Dec-2017)_Neat
P. 3
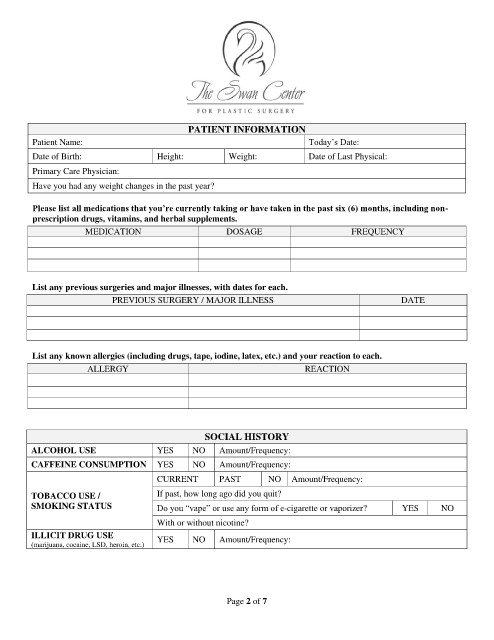
PATIENT INFORMATION
Patient Name: Today’s Date:
Date of Birth: Height: Weight: Date of Last Physical:
Primary Care Physician:
Have you had any weight changes in the past year?
Please list all medications that you’re currently taking or have taken in the past six (6) months, including non-
prescription drugs, vitamins, and herbal supplements.
MEDICATION DOSAGE FREQUENCY
List any previous surgeries and major illnesses, with dates for each.
PREVIOUS SURGERY / MAJOR ILLNESS DATE
List any known allergies (including drugs, tape, iodine, latex, etc.) and your reaction to each.
ALLERGY REACTION
SOCIAL HISTORY
ALCOHOL USE YES NO Amount/Frequency:
CAFFEINE CONSUMPTION YES NO Amount/Frequency:
CURRENT PAST NO Amount/Frequency:
TOBACCO USE / If past, how long ago did you quit?
SMOKING STATUS Do you “vape” or use any form of e-cigarette or vaporizer? YES NO
With or without nicotine?
ILLICIT DRUG USE YES NO Amount/Frequency:
(marijuana, cocaine, LSD, heroin, etc.)
Page 2 of 7