Page 138 - Business Development Orientation Binder
P. 138
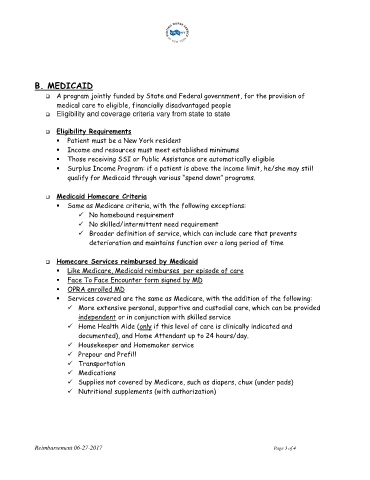
B. MEDICAID
A program jointly funded by State and Federal government, for the provision of
medical care to eligible, financially disadvantaged people
Eligibility and coverage criteria vary from state to state
Eligibility Requirements
Patient must be a New York resident
Income and resources must meet established minimums
Those receiving SSI or Public Assistance are automatically eligible
Surplus Income Program: if a patient is above the income limit, he/she may still
qualify for Medicaid through various “spend down” programs.
Medicaid Homecare Criteria
Same as Medicare criteria, with the following exceptions:
No homebound requirement
No skilled/intermittent need requirement
Broader definition of service, which can include care that prevents
deterioration and maintains function over a long period of time
Homecare Services reimbursed by Medicaid
Like Medicare, Medicaid reimburses per episode of care
Face To Face Encounter form signed by MD
OPRA enrolled MD
Services covered are the same as Medicare, with the addition of the following:
More extensive personal, supportive and custodial care, which can be provided
independent or in conjunction with skilled service
Home Health Aide (only if this level of care is clinically indicated and
documented), and Home Attendant up to 24 hours/day.
Housekeeper and Homemaker service
Prepour and Prefill
Transportation
Medications
Supplies not covered by Medicare, such as diapers, chux (under pads)
Nutritional supplements (with authorization)
Reimbursement 06-27-2017 Page 3 of 4