Page 59 - Rehab 2020
P. 59
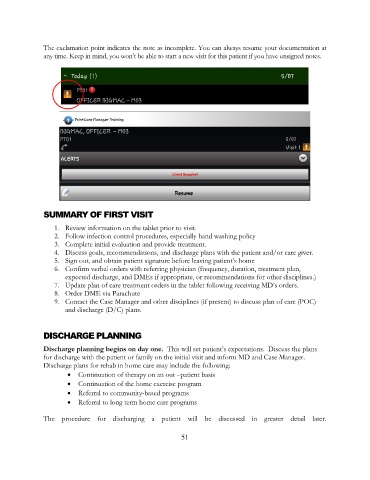
The exclamation point indicates the note as incomplete. You can always resume your documentation at
any time. Keep in mind, you won’t be able to start a new visit for this patient if you have unsigned notes.
SUMMARY OF FIRST VISIT
1. Review information on the tablet prior to visit.
2. Follow infection control procedures, especially hand washing policy
3. Complete initial evaluation and provide treatment.
4. Discuss goals, recommendations, and discharge plans with the patient and/or care giver.
5. Sign out, and obtain patient signature before leaving patient’s home
6. Confirm verbal orders with referring physician (frequency, duration, treatment plan,
expected discharge, and DMEs if appropriate, or recommendations for other disciplines.)
7. Update plan of care treatment orders in the tablet following receiving MD’s orders.
8. Order DME via Parachute
9. Contact the Case Manager and other disciplines (if present) to discuss plan of care (POC)
and discharge (D/C) plans.
DISCHARGE PLANNING
Discharge planning begins on day one. This will set patient’s expectations. Discuss the plans
for discharge with the patient or family on the initial visit and inform MD and Case Manager.
Discharge plans for rehab in home care may include the following:
• Continuation of therapy on an out –patient basis
• Continuation of the home exercise program
• Referral to community-based programs
• Referral to long term home care programs
The procedure for discharging a patient will be discussed in greater detail later.
51