Page 167 - Basic Monitoring in Canine and Feline Emergency Patients
P. 167
D3 converted to 25-
1-α
Vitamin Absorbed GI tract hydroxycholecalciferol hydroxylase (–) ↑ P
D3
VetBooks.ir (dietary) [in liver] [in kidney]
FGF-23 (–)
(–) 25-hydroxycholecalciferol
↑ Parathyroid converted to Calcitriol
hormone (–)
Release Ca (and [active form vitamin D]
phosphorus) from (–)
bone
Absorbs Ca
(and
phosphorus)
(–)
↓ Serum Increase reabsorption Ca (and excretion from GI
calcium phosphorus) [kidney tubule] tract
levels
↑ Serum calcium
levels
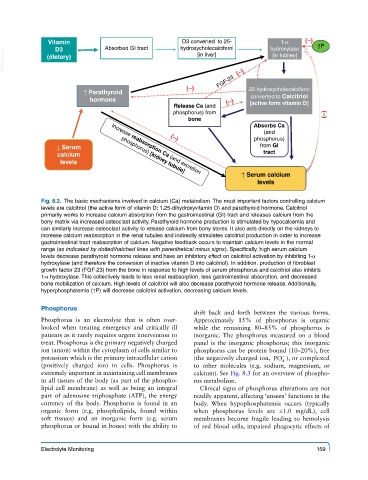
Fig. 8.2. The basic mechanisms involved in calcium (Ca) metabolism. The most important factors controlling calcium
levels are calcitriol (the active form of vitamin D; 1,25-dihydroxyvitamin D) and parathyroid hormone. Calcitriol
primarily works to increase calcium absorption from the gastrointestinal (GI) tract and releases calcium from the
bony matrix via increased osteoclast activity. Parathyroid hormone production is stimulated by hypocalcemia and
can similarly increase osteoclast activity to release calcium from bony stores. It also acts directly on the kidneys to
increase calcium reabsorption in the renal tubules and indirectly stimulates calcitriol production in order to increase
gastrointestinal tract reabsorption of calcium. Negative feedback occurs to maintain calcium levels in the normal
range (as indicated by dotted/hatched lines with parenthetical minus signs). Specifically, high serum calcium
levels decrease parathyroid hormone release and have an inhibitory effect on calcitriol activation by inhibiting 1-α
hydroxylase (and therefore the conversion of inactive vitamin D into calcitriol). In addition, production of fibroblast
growth factor 23 (FGF-23) from the bone in response to high levels of serum phosphorus and calcitriol also inhibits
1-α hydroxylase. This collectively leads to less renal reabsorption, less gastrointestinal absorption, and decreased
bone mobilization of calcium. High levels of calcitriol will also decrease parathyroid hormone release. Additionally,
hyperphosphatemia (↑P) will decrease calcitriol activation, decreasing calcium levels.
Phosphorus
shift back and forth between the various forms.
Phosphorus is an electrolyte that is often over- Approximately 15% of phosphorus is organic
looked when treating emergency and critically ill while the remaining 80–85% of phosphorus is
patients as it rarely requires urgent intervention to inorganic. The phosphorus measured on a blood
treat. Phosphorus is the primary negatively charged panel is the inorganic phosphorus; this inorganic
ion (anion) within the cytoplasm of cells similar to phosphorus can be protein bound (10–20%), free
−
potassium which is the primary intracellular cation (the negatively charged ion, PO ), or complexed
4
(positively charged ion) in cells. Phosphorus is to other molecules (e.g. sodium, magnesium, or
extremely important in maintaining cell membranes calcium). See Fig. 8.3 for an overview of phospho-
in all tissues of the body (as part of the phospho- rus metabolism.
lipid cell membrane) as well as being an integral Clinical signs of phosphorus alterations are not
part of adenosine triphosphate (ATP), the energy readily apparent, affecting ‘unseen’ functions in the
currency of the body. Phosphorus is found in an body. When hypophosphatemia occurs (typically
organic form (e.g. phospholipids, found within when phosphorus levels are ≤1.0 mg/dL), cell
soft tissues) and an inorganic form (e.g. serum membranes become fragile leading to hemolysis
phosphorus or bound in bones) with the ability to of red blood cells, impaired phagocytic effects of
Electrolyte Monitoring 159