Page 7 - Remita Guide 2020 - CA FINAL
P. 7
Changes to enrollment
Open Enrollment
During our annual open enrollment period, you may make new benefit elections for the following January 1st effective
date.
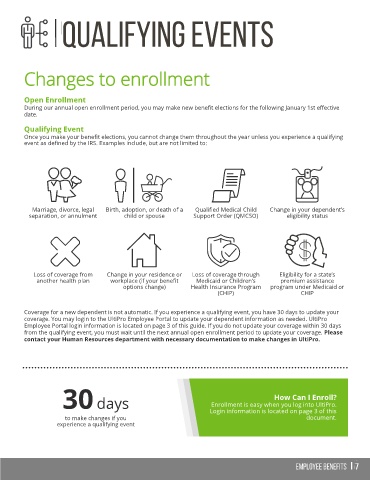
Qualifying Event
Once you make your benefit elections, you cannot change them throughout the year unless you experience a qualifying
event as defined by the IRS. Examples include, but are not limited to:
Marriage, divorce, legal Birth, adoption, or death of a Qualified Medical Child Change in your dependent’s
separation, or annulment child or spouse Support Order (QMCSO) eligibility status
Loss of coverage from Change in your residence or Loss of coverage through Eligibility for a state’s
another health plan workplace (if your benefit Medicaid or Children’s premium assistance
options change) Health Insurance Program program under Medicaid or
(CHIP) CHIP
Coverage for a new dependent is not automatic. If you experience a qualifying event, you have 30 days to update your
coverage. You may login to the UltiPro Employee Portal to update your dependent information as needed. UltiPro
Employee Portal login information is located on page 3 of this guide. If you do not update your coverage within 30 days
from the qualifying event, you must wait until the next annual open enrollment period to update your coverage. Please
contact your Human Resources department with necessary documentation to make changes in UltiPro.
How Can I Enroll?
30 days Enrollment is easy when you log into UltiPro.
Login information is located on page 3 of this
to make changes if you document.
experience a qualifying event