Page 6 - OrangeTheory Benefits Guide 07-2019_FINAL
P. 6
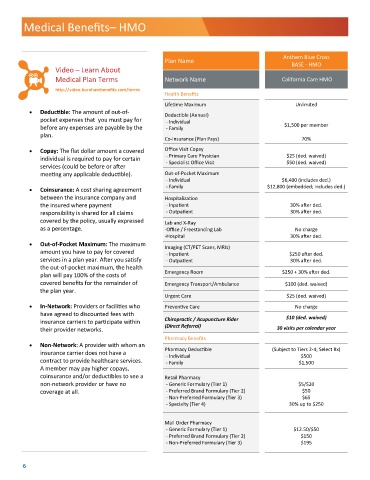
Medical Benefits– HMO
Anthem Blue Cross
Plan Name
BASE - HMO
Video – Learn About
Medical Plan Terms Network Name California Care HMO
http://video.burnhambenefits.com/terms
Health Benefits
Lifetime Maximum Unlimited
• Deductible: The amount of out-of-
Deductible (Annual)
pocket expenses that you must pay for - Individual
before any expenses are payable by the - Family $1,500 per member
plan.
Co-Insurance (Plan Pays) 70%
• Copay: The flat dollar amount a covered Office Visit Copay
- Primary Care Physician $25 (ded. waived)
individual is required to pay for certain
- Specialist Office Visit $50 (ded. waived)
services (could be before or after
meeting any applicable deductible). Out-of-Pocket Maximum
- Individual $6,400 (includes ded.)
• Coinsurance: A cost sharing agreement - Family $12,800 (embedded; includes ded.)
between the insurance company and Hospitalization
the insured where payment - Inpatient 30% after ded.
responsibility is shared for all claims - Outpatient 30% after ded.
covered by the policy, usually expressed Lab and X-Ray
as a percentage. -Office / Freestanding Lab No charge
-Hospital 30% after ded.
• Out-of-Pocket Maximum: The maximum
Imaging (CT/PET Scans, MRIs)
amount you have to pay for covered - Inpatient $250 after ded.
services in a plan year. After you satisfy - Outpatient 30% after ded.
the out-of-pocket maximum, the health
plan will pay 100% of the costs of Emergency Room $250 + 30% after ded.
covered benefits for the remainder of Emergency Transport/Ambulance $100 (ded. waived)
the plan year.
Urgent Care $25 (ded. waived)
• In-Network: Providers or facilities who Preventive Care No charge
have agreed to discounted fees with $10 (ded. waived)
insurance carriers to participate within Chiropractic / Acupuncture Rider
(Direct Referral)
their provider networks. 30 visits per calendar year
Pharmacy Benefits
• Non-Network: A provider with whom an
Pharmacy Deductible (Subject to Tiers 2-4; Select Rx)
insurance carrier does not have a - Individual $500
contract to provide healthcare services. - Family $1,500
A member may pay higher copays,
coinsurance and/or deductibles to see a Retail Pharmacy
non-network provider or have no - Generic Formulary (Tier 1) $5/$20
coverage at all. - Preferred Brand Formulary (Tier 2) $50
- Non-Preferred Formulary (Tier 3) $65
- Specialty (Tier 4) 30% up to $250
Mail Order Pharmacy
- Generic Formulary (Tier 1) $12.50/$50
- Preferred Brand Formulary (Tier 2) $150
- Non-Preferred Formulary (Tier 3) $195
6